As a champion of wellness care like you, I strongly believe in the principles of building musculoskeletal health over time through chiropractic care. The simple truth, however, is that most patients who are placed in wellness care plans do not belong there.
Helping Your Patients Achieve True Musculoskeletal Wellness: Are You Doing Enough?
Evaluating the structural mechanics of a patient from the ground up is vital to discovering the underlying cause of postural imbalance, instability and unstable conditions requiring ongoing symptom-based care. Without understanding and appreciating commonly overlooked structural abnormalities and how they affect body mechanics though the kinetic chain reaction, it is impossible to achieve musculoskeletal wellness for our patients.
I spent several years in practice "looking to the spine for the cause of disease," but have realized I may have been reading the wrong ancient philosopher. Leonardo da Vinci observed that "the human foot is a masterpiece of engineering and a beautiful work of art." In practice, I rarely encounter a patient who does not have some level of clinically significant, permanent, structural foot or other lower extremity imbalance.
As one of the primary structural components of foundational body mechanics, the foot is vital to achieving musculoskeletal wellness.
Identifying Adaptive Symptoms
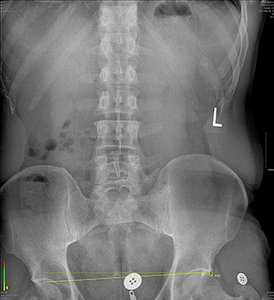 FIG 1 Barefoot standing X-ray.
All that being said, the human body has an amazing ability to adapt. These underlying conditions can be present for years without sign or symptom. However, each body reaches its limit at some point. This sudden failure to adapt can occur due to trauma, a sudden increase in mechanical stress or mechanical stress being applied consistently over time. Whatever the case may be, the result is a symptom.
FIG 1 Barefoot standing X-ray.
All that being said, the human body has an amazing ability to adapt. These underlying conditions can be present for years without sign or symptom. However, each body reaches its limit at some point. This sudden failure to adapt can occur due to trauma, a sudden increase in mechanical stress or mechanical stress being applied consistently over time. Whatever the case may be, the result is a symptom.
On the other hand, the symptoms may have been present for years and years in the form of low back pain, but no one made the connection between lower extremity mechanics and the low back. How many chiropractic patients are treated for weeks, months and years for LBP without ever being evaluated for a clinically significant structural imbalance?
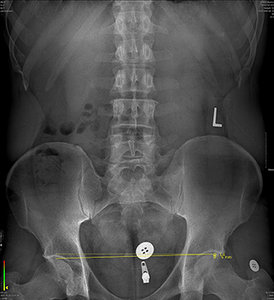 FIG 2 Standing X-ray with bilateral custom orthotic support.
Sadly, the majority of these patients, after being adjusted, are back in to the same adaptational situation that is leading to low back pain before even making it back to their car.
FIG 2 Standing X-ray with bilateral custom orthotic support.
Sadly, the majority of these patients, after being adjusted, are back in to the same adaptational situation that is leading to low back pain before even making it back to their car.
Some common symptoms associated with lower extremity structural imbalances are: foot, knee, hip and low back pain. Finding relief from these symptoms can be achieved with musculoskeletal treatment and activity modification; but frequently, these symptoms are persistent due to excessive, uneven tissue loading, resulting in repetitive-stress injury.
Clinical Case Studies to Consider
Case #1: A 27-year-old male presenting with right knee and hip pain midway through a marathon training schedule.
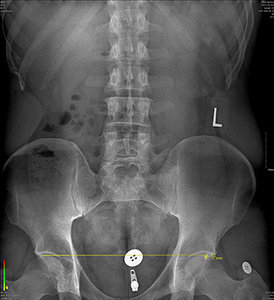 FIG 3 Standing X-ray with bilateral orthotic support and 6 mm heel lift on right.
No history of trauma was reported, but pain in the right knee and hip were only experienced upon running 10 miles or more.
FIG 3 Standing X-ray with bilateral orthotic support and 6 mm heel lift on right.
No history of trauma was reported, but pain in the right knee and hip were only experienced upon running 10 miles or more.
There was an unremarkable orthopedic exam. Digital laser scan of the plantar vault revealed symmetrical lateral arch collapse. In addition, an apparent 14 mm reduction deficit was noted in the right femur upon X-ray.
The patient was fitted with custom three-arch foot orthotics and lumbopelvic X-rays were repeated. With the orthotics, the actual reduction deficit in the right femur was measured at 6 mm. A 6 mm heel lift was added on the right and follow-up X-ray revealed a zero-deficit femoral head height measurement.
With ancillary treatment for symptomatic relief and a slow progression in running mileage, the patient was returned to marathon training with full condition resolution.
Case #2: A 42-year-old female presenting with non-traumatic, constant low back pain.
Orthopedic exam was generally unremarkable. Digital laser scan of the plantar vault revealed asymmetrical arch collapse in the right lateral and transverse arches totaling 4.2 mm. Additionally, an apparent 6 mm reduction deficit was measured in the right femur.
The patient was fitted with custom three-arch foot orthotics and lumbopelvic X-rays were repeated. With the orthotics, the actual reduction deficit in the right femur was measured at 1 mm and well under the clinically significant 3 mm benchmark.
The patient was additionally treated for three weeks for low back pain. Successful integration into the orthotics was achieved and full resolution was reported by the patient.
These two cases represent a small example in a much larger cohort. In their recent publication, Tim Maggs, et al., report: "Custom orthotics are necessary to avoid further collapse of the foot arches, but, often significant biomechanical imbalances occurs and remain unidentified and untreated. It's only when we look at the body as an interconnected biomechanical structure that we are then able to identify and work to improve biomechanical imbalances that produce musculoskeletal injuries."1
We Must Refuse to Be Just a Musculoskeletal Band-Aid
The question then remains: Can we appropriately diagnose and treat musculoskeletal conditions without accurately analyzing structural body mechanics from the ground up? It is true that some conditions require maintenance. However, disease maintenance is a page from the allopathic playbook. If we are going to transcend the trap of condition management and become true wellness providers, we must refuse to remain a musculoskeletal Band-Aid, and actually identify and correct the underlying causes.
Reference
- Maggs T, et al. When correcting the collapse of arches of the feet with custom orthotics, are other areas of the body effected? A revolutionary approach towards reduced injuries and better outcomes. Ortho & Rheum Open Access J, 2020;17(1):555953.
Dr. Scott Saario is a graduate of the University of the State of New York and Palmer College of Chiropractic. He is the owner of ChiroCabarrus in Concord, N.C., and focuses on sports biomechanics and prevention of athletic injuries. He can be reached with questions and comments at
.




