The facet syndrome can be a difficult disorder to manage and even diagnose. This disorder can be associated with clinical symptoms that simulate a disc lesion. Radiographic findings may not confirm the diagnosis.
The term "facet syndrome" generally is associated with an overriding of the facets of the adjacent vertebrae. The facets have been implicated as a source of low back pain as early as 1911, reported by Goldthwait,2 who stated that the anomalous placement of the facets could be a cause for symptoms. In 1933, Ghormley reported that the facets could be a cause of sciatic pain.3
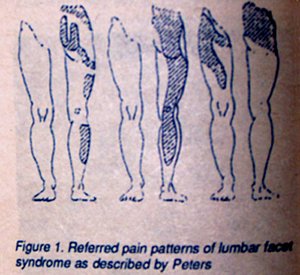
Clinically, the patient with a typical facet syndrome will complain of a sudden onset of unilateral or bilateral low back pain -- with or without sciatic radiation. The referred pain pattern will differ depending on which facets are the cause of the symptoms.
The pain generally increases with motion, particularly with extension, and is relieved by rest. Facet pain, unlike disc pain, is not increased by coughing or sneezing.
Localized tenderness usually is observed at the lumbosacral junction and a "spring test" of the individual facets often will reproduce the pain. The "spring test" can be performed by palpating the facet joint and pressing initially down on the facet with deep pressure, then releasing quickly.1 Kleynhans4 has classified facet syndrome into three types.
1. Traumatic type: due to injury to the facet joint and associated with inflammation to the joint capsule.
2, Pathologic type: due to degenerative arthrosis of the facet joint and generally associated with degenerative disc disease.
3. Postural type: due to biomechanical changes that place more stress upon the facets, i.e., chronic occupational strain and overweight.
In general, the radiographic findings of facet imbrication or overriding of the facets is indicative of a possible facet syndrome. Macnab's joint body line can also be used as a radiographic indication of disc thinning and facet imbrication.5
The sacral base angle is also helpful when one suspects a possible facet syndrome at the L5/S1 level.6
It has also been suggested that a posterior shift in the Ferguson's gravity line may predispose a patient to a facet syndrome involving the lumbosacral junction.7 Erhardt and Hildebrandt have referred to an abnormal lumbosacral disc angle measurement may be an indication of a facet syndrome.8,9 Cox and Erhardt have stated that the facet syndrome angle changes can be associated with a facet syndrome in the lumbosacral region.10
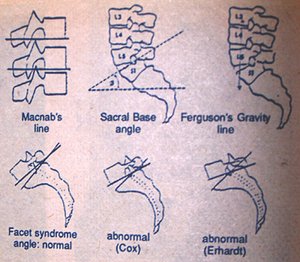
An increase in the sacral base angle and lumbosacral disc angle, and a posterior shift in the gravity line all suggest the tendency toward a facet syndrome. Generally, most patients with an uncomplicated facet syndrome will respond to chiropractic adjustments as long as the correct level is mobilized.11
References
- Peters, R.E. "Facet Syndrome." European Journal of Chiropractic 1984.
- Goldthwait, J.E. "The Lumbosacral Articulation: an explanation of many cases of 'lumbago,' 'sciatica,' and 'paraplegia.'" Boston Medical Surgical Journal 1911.
- Ghormley, R.K. "Low Back Pain with Special Reference to the Articular Facets, with Presentation of An Operative Procedure." Journal of American Medical Association 1933.
- Kleynhans, A.M. "Facet Syndrome." Journal of the Austrian Chiropractic Association, 1976.
- Macnab, I. "Backache." William and Wilkins 1977.
- Keats, T; Lusted, L. "Atlas of Roentgenographic Measurement." Year-Book Medical Publishers 1985.
- Ferguson, A.B. "Roentgen Diagnosis of Extremities and Spine." New York, Paul B. Hoeber 1949.
- Erhardt, R.; "Erhardt X-ray Seminar Notes." Erhardt, Dunwoody, George 1976.
- Hildebrandt, R.W. "Chiropractic Spinography." Hilmark Publications 1977.
- Cox, J.M. "The Facet Syndrome." Digest Chiropractic Economics 1980.
- Banks, S.D. "Lumbar Facet syndrome: Spinographic Assessment of Treatment by Spinal Manipulative Therapy." Journal of Manipulative and Physiological Therapeutics December 1983.
Click here for more information about Deborah Pate, DC, DACBR.





