I am always trying to be as specific as I can in my lower back diagnosis. At the same time, there are common patterns (like this one) that seem to impact multiple problems and diagnoses. Gluteus medius weakness can contribute to lateral hip pain, buttock pain, low back pain and/or stresses on the knee.
Let's focus on inhibition / weakness of the lateral system, including the gluteus medius, as well as the gluteus minimus and the TFL.
Potential Consequences
What happens when the lateral supportive musculature is not up to par? The hip shifts laterally to the involved side, with a contralateral drop of the opposite-side pelvis with every step you take. This is a compensated Trendelenburg gait. The frontal-plane muscles are not adequate to support the unilateral weight-bearing in gait, on stance phase.
Consider an example of left-side weakness / inhibition. Up the chain, when the right side of the pelvis drops, the lumbar spine becomes concave and compressed on the left with every step. The foot and knee mechanics will be compromised, with either a valgus stress to the knee or in some, a bowlegged stance with a wide gait, with varus stress to the knee. There are likely to be compensations all the way up to the top of the spine.
Possible Pain Mechanisms
Let's look at various pain mechanisms. In all of these patterns, you have a vicious cycle of pain and weakness reinforcing each other.
- Any chronic unilateral lower back or pelvic pain will create one-sided inhibition of the core musculature, including the glutes.
- The patient will end up with a overstretch of the lateral structures on the ipsilateral side. This can be called trochanteric bursitis; although the term is usually inaccurate.
- The lumbar spine, both facets and discs, are being compressed on the concave side of the curve with every step. This can cause facet- or disc-generated pain.
- Nerve impingements (deep gluteal syndrome) affect the superior gluteal nerve as it exits just above the piriformis. This nerve, from L5, S1 and S2, supplies the gluteus medius. This one is new to me, so I won't try to explain the concept. Justin Dean and Phillip Snell have a detailed blog post about the superior gluteal nerve.
- Sensory nerve impingements (Maigne syndrome), such as irritation of the ilio-hypogastric nerve, lateral branch, coming from L1 and L2. This nerve supplies sensation to the skin over the lateral buttock.
Identifying the Lateral Weakness
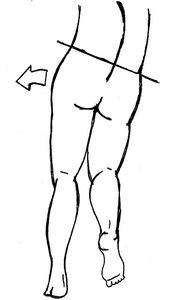 An exaggerated view of the left gluteus medius failure pattern.
How can you identify this pattern of lateral weakness? First, as chiropractors, we are usually looking at functional patterns. This weakness or inhibition is unlikely to show up on a nerve conduction study. The gluteus medius weakness may or may not be apparent on manual muscle testing.
An exaggerated view of the left gluteus medius failure pattern.
How can you identify this pattern of lateral weakness? First, as chiropractors, we are usually looking at functional patterns. This weakness or inhibition is unlikely to show up on a nerve conduction study. The gluteus medius weakness may or may not be apparent on manual muscle testing.
If you have good visual skills, you could use gait analysis, perhaps aided by a treadmill, or a slow-motion video on your smartphone. You are looking for two aberrant movements: the hip and pelvis shifting toward the weak side, and the pelvis dropping on the opposite side. I'm not as good at watching movement, so I use other functional tests. Have the patient load the involved side, and watch the PSIS movement from behind.
Stand behind the patient. Place both of your thumbs at the bottom of the PSISs. Have the patient step forward on their left leg, load that leg, and then stop with the left leg forward in their normal gait stance. If the right PSIS is now lower than the left, you have documented frontal-plane failure on the left. Test the other side to compare.
Another test involves having the patient do a mini squat on the left leg, bending the left knee 10-20 degrees. The right leg is lifted an inch or two and is non-weight-bearing. The patient will tend to be less stable on the weak side. The ipsilateral knee will often drive medially because the hip abductors cannot pull the knee in line over the toes. You'll see a similar visual, with the pelvis shifting left and the right side of the pelvis dropping.
I like to palpate for weakness and atrophy. I check the QL, as well as the lateral portion of the oblique abdominals and the gluteus medius. To me, the QL weakness is more obvious as a "gushy" soft feel compared to the opposite side.
Palpate both the upper lumbar and the lower lumbar joints for fixation. Palpate the courses of the involved nerves for sensitivity. Check and correct hip motion. What muscles have tissue texture changes?
Manual and Other Corrections
What is the correction? Start with rehab. Good rehab is not just exercises. Good rehab is attempting to change deep, old patterns. Good rehab is often unilateral or focused on a specific side. The ideal patient will tune in to their old patterns and try to change them with every step they take.
What exercises are useful? The clamshell is useful to wake up the glutes. Remember that the clamshell is not primarily for strength, but to teach the patient to differentiate between hip and pelvic motions.
The side step, AKA lateral band walk or monster walk, is another great one. It is functional and weight-bearing. Place the band just above the knee. (As this exercise gets easier, place the band lower on the leg.) The emphasis is on the left stability leg, pushing out with the right leg.
The patient needs to maintain an athletic stance / shortstop squat. After 10 to 20 steps, the patient will usually begin to feel the fatigue in the left glutes. Ideally, they need to quit leaking; to consciously stop the left pelvic side shift when they begin to lift the right leg.
Other gluteal exercises, such as one-leg bridges and/or single-leg deadlifts, also challenge the entire gluteal complex. Functionally, we cannot isolate one muscle; we are trying to improve a movement pattern.
Manual therapies can help break the cycle. Correct joint dysfunctions: the upper lumbar, affecting the cluneal complex nerves; the lower lumbar/SI (with referral into the buttocks); and the hip joint. For irritated nerves, consider Dermal Traction Method or neurodynamic approaches. Are there fascial restrictions in the region? You probably have plenty of fascial release tools.
After 40 years of practice, I am never bored. A challenging lower back problem keeps my brain going. I hope I can inspire you to feel that.
Author's Note: Special thanks to my colleagues: Dan Loch, DPT (who pointed out this pattern to me in my own body); Phillip Snell and Justin Dean of Dermal Traction and the Neuro-Centric model; and Nate Crider, MD, and Bill Esser, PT, for biomechanics and editing help).
Click here for more information about Marc Heller, DC.





