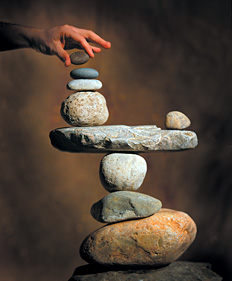
You already know how complicated the process of human balance is; but are you aware of the simple tools many providers are using to improve their patients' balance? Balance requires coordinated participation of the sensory (visual, vestibular and proprioceptive) and motor systems.
Interesting evidence demonstrates the intimate relationship between vision and posture. For example, a study of 160,000 school-aged children linked minor vision abnormalities with consistent patterns of postural distortions – including head tilts and rotations, changes in the cervical lordosis, and rotational scapular misalignments.2 Furthermore, chiropractic adjustments to the upper cervical spine alone were shown to improve visual imbalances in a study of 25 patients.3
Inputs and Resources
Obviously, a referral is appropriate if potential vision problems are contributing to subluxation formation. On the other hand, the chiropractor's ability to positively affect proprioception and motor control should be fairly obvious. As Yochum and Maggs have recently pointed out, the chiropractic profession is "the most equipped to both detect and improve biomechanical fixations and imbalances."4 Let's examine the mechanism whereby balance in the standing posture can be improved, highlighting resources available to the chiropractor in addition to adjustments.
 Proprioception is the summation of various inputs from mechanoreceptors found in joint capsules, ligaments, muscles, tendons, and skin.2 Motor control initiates an appropriate muscular response to the combined visual and proprioceptive inputs, completing the feedback loop and providing a series of finely tuned adjustments, leading to postural balance.
Proprioception is the summation of various inputs from mechanoreceptors found in joint capsules, ligaments, muscles, tendons, and skin.2 Motor control initiates an appropriate muscular response to the combined visual and proprioceptive inputs, completing the feedback loop and providing a series of finely tuned adjustments, leading to postural balance.
While erect, the multi-linked human structure is very dynamic. However, there is a limit to the amount of A-P and lateral sway permitted by the foundation before an individual is forced to either correct their posture or stumble. The limit is fairly consistent among individuals and is proportional to the plantar surface area of the feet compared to physical height. I will refer to this limit as the "stability field."
Fields and Patterns
Under normal circumstances, the stability field is much broader than normal patterns of sway in healthy individuals. A sway pattern is most efficient when it is concentrated around the individual's center of gravity. The closer a person's sway pattern is to the edge of their stability field, the more likely they will suffer from muscular fatigue and degenerative conditions, not to mention fall. In order to maximize balance, the practitioner must focus attention on increasing the stability field and decreasing, or stabilizing, the patient's sway pattern.
Injuries to the lower extremity, whether acute or from chronic deformation, can alter proprioception and diminish the motor response of balance.1 According to Nashner, et al., any musculoskeletal abnormality – for example, weakness of the ankle joint muscles and/or reduced range of motion about the ankles – shrinks the limits of stability.5
Because the center of gravity is near the lower abdomen, we rely on two major balance strategies involving the lower extremities: an ankle strategy and a hip strategy. The body can use either strategy or a combination of the two, depending on the circumstances. Simply stated, small, corrective movements at these joints produce balance. However, when the feet are unstable, the ankle strategy is unable to maintain balance, and overutilization of hip muscles and joints occurs. The ankle strategy is most effective when the sway pattern is small and very near the center of gravity.5
The ankle strategy requires adequate range of motion and muscle strength about the ankles, a firm and secure support base, and the ability to sense the support base.5 It's not surprising, then, that individually designed stabilizing orthotics are a key adjunct to this strategy, because such orthotics support normal range of motion; provide structural support and joint alignment; and maximize proprioceptive feedback for muscular stability and coordination.
The Orthotic Effect
Many adults are faced with cumulative traumas, combined with the degenerative conditions of ligament laxity and decreased afferent input in general. Research suggesting that stabilizing orthotics enhance balance and proprioception is very encouraging. Stude, Brink and Gullickson demonstrated that experienced golfers, after wearing stabilizing orthotics daily for a period of six weeks, showed improvements in balance and proprioception.6-8 This becomes significant given the fact that experienced golfers would be expected to have maximized their coordination and balance abilities as it relates to the game of golf. However, the orthotics had the effect of broadening the stability field while focusing the sway pattern around the center of gravity.
Chiropractic adjustments improve proprioceptive input by normalizing joint alignment and muscle tonus in general. Adjustments are most effective when supported by proper muscular retraining, rehabilitation and orthotic support. The feet contain approximately one-quarter of all the body's joints and a concentration of proprioceptive fibers. Therefore, it makes sense that supporting the postural foundation using individually designed, stabilizing orthotics will help enhance balance.
References
- Irrgang JJ, Whitney SL, Cox ED. Balance and proprioceptive training for rehabilitation of the lower extremity. J Sport Rehab, 1994;3:68-83.
- Harmon, DB. Notes on a Dynamic Theory of Vision. Austin, TX: self published, 1958.
- Sutton, AA. Building a Visual Space World, Curriculum II. Santa Ana, CA: Optometric Extension Program Foundation, 1984.
- Yochum TR, Maggs T. "100% of My Patients Get Custom Orthotics: What About Yours?" The American Chiropractor, 2011;33(8):26-34.
- Nashner LM, Shupert CL, Horak FB, Black FO. Organization of posture controls: an analysis of sensory and mechanical constraints. Prog Brain Res, 1989;80:411-418.
- Stude DE, Brink DK. Effects of nine holes of simulated golf and orthotics intervention on balance and proprioception in experienced golfers. J Manip Physiol Ther, 1997;20(9):590-601.
- Stude DE, Gullickson J. Effects of orthotic intervention and nine holes of simulated golf on gait in experienced golfers. J Manip Physiol Ther, 2001;24(4):279-287.
- Stude DE, Gullickson J. Effects of orthotic intervention and nine holes of simulated golf on club-head velocity in experienced golfers. J Manip Physiol Ther, 2000;23(3):168-174.
Click here for previous articles by Mark Charrette, DC.





