The arcuate foramen is an underestimated structure that clinically, has been associated with tethering of the vertebral artery and dissection from repetitive trauma with movement of the neck.
Clinicians should consider the possibility of an arcuate foramen with patients complaining of vertigo, headache, shoulder-arm and neck pain. Cervical spine radiography is a simple and useful technique to determine the presence of arcuate foramen. (Figure 1)
There is some debate as to the actual nature of the arcuate foramen. Is it due to calcification or ossification of the posterior atlanto-occipital ligament, or is a vestigial structure? Regardless of its origin, the ossified structure bridges from the posterior aspects of the lateral mass of atlas to the posterior arch, forming a bony arch called the arcuate foramen. When present, the vertebral artery and the dorsal rami of the first cervical nerve traverse through the foramen as they pass over the posterior arch to enter and exit the foramen magnum, respectively.
Several other phrases have been used to describe the arcuate foramen, including posterior ponticle, Kimmerle anomaly, foramen arcuate, pons ponticus and ponticulus ponticus.
Anatomy of the Vertebral Artery
 Figure 1: Cervical X-ray of the arcuate foramen. The portion of the radiograph showing the structure has been enlarged at top right for viewing.
Anatomically, the course of the vertebral artery is a difficult one: It arises from the subclavian artery and ascends posterior to the internal carotid artery in the transverse foramina of the cervical vertebrae, terminating with the contralateral vertebral artery to form the basilar artery.
Figure 1: Cervical X-ray of the arcuate foramen. The portion of the radiograph showing the structure has been enlarged at top right for viewing.
Anatomically, the course of the vertebral artery is a difficult one: It arises from the subclavian artery and ascends posterior to the internal carotid artery in the transverse foramina of the cervical vertebrae, terminating with the contralateral vertebral artery to form the basilar artery.
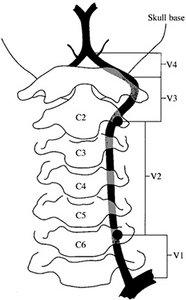
The vertebral artery can be divided into three extracranial segments and an intracranial portion. (Figure 1) Segment one is from the origin to the point at which it enters the transverse foramina of either the fifth or sixth cervical vertebra. In segment two, it courses within the transverse foramina until exiting as the third segment behind the atlas and heading toward the foramen magnum.
The final intracranial portion begins as it pierces the dura and arachnoid mater at the base of the skull, and ends as it meets its opposite vertebral artery to form the midline basilar artery at the level of the medullopontine junction. In its extracranial portion, the vertebral artery gives small spinal branches to the periosteum and vertebral bodies, and muscular branches to the deep surrounding muscles of the region.
The short intracranial segment gives off major anterior and posterior spinal arteries to the medulla and spinal cord, minute penetrating vessels to the medulla and its largest branch – the posterior inferior cerebellar artery (PICA), which supplies a small portion of the dorsal medulla and cerebellum.
As it enters the skull, the vertebral artery wall shows marked reduction in the thickness of the adventitial and medial layers, and a reduction of elastic fibers in the media and external elastic lamina. In up to 15 percent of the healthy population, one vertebral artery is atretic (<2 mm diameter) and makes little contribution to basilar artery flow. Lesser degrees of asymmetry are also common.
The left vertebral artery is dominant in approximately 50 percent; the right in 25 percent; and only in the remaining quarter of cases are the two vertebral arteries of similar caliber.
Complications and Symptoms
The most common disease affecting the vertebral artery is atherosclerosis. Atherosclerotic stenosis most commonly affects the first portion of the vertebral arteries or extends from plaques that compromise the origin of the vertebral arteries as they arise from the brachiocephalic and subclavian arteries. Lesions at the midportion of the vertebral arteries can occur when overgrowth of the transverse process of a vertebra impinges on the artery as it passes through the bony canal.
In such cases, symptoms are commonly provoked by head turning, during which an osteophyte obstructs the vertebral artery. Symptoms associated with vertebral artery occlusive disease include dizziness, vertigo, diplopia, perioral numbness, blurred vision, tinnitus, ataxia, bilateral sensory deficits, and syncope, all of which can be caused by other disease entities, including cardiac arrhythmias, orthostatic hypotension, and vestibular disorders.
Chiropractic Significance
Knowledge of the anatomic relationship of the vertebral artery and the arcuate foramen is important for the chiropractor when considering cervical manipulation, especially if the patient has clinical symptoms that might indicate osseous compromise of the vertebral artery.
Complaints of occipital headaches, vertigo, pain in the temporal region, pain in the back of the eye, periodic photophobia, paraesthesia of hands or sensation of pressure on hands with thepresence of an arcuate foramen should be considered a red flag. Even though the above-mentioned symptoms do not occur in a majority of patients with a posterior ponticle, precautions should nevertheless be undertaken to minimize the risk of complications to the patient.
Start To Finish: The Vertebral Artery
 The vertebral artery is typically
divided into four segments:
The vertebral artery is typically
divided into four segments:
- V1: origin to the transverse foramen of C6
- V2: transverse foramen of C6 to the transverse foramen of C2
- V3: C2 to the dura
- V4: from the dura to their confl uence to form the basilar artery
V1 angles posteriorly between the longus colli medially and scalenus anterior laterally behind the common carotoid artery to enter the transverse foramen of C6.
Relations:
- Anteriorly: common carotid artery, vertebral vein, thoracic duct (left VA, and lymphatic duct (right VA)
- Posteriorly: ventral rami of C7 and C8, transverse process of C7, inferior cervical ganglion
- Anteromedially: inferior thyroid artery, middle cervical ganglion
V2 passes through the transverse foramina of the cervical vertebrae, normally C6-C2. Here it is accompanied by vertebral veins and sympathetic nerves.
V3 emerges from the transverse process of C2 (axis) and sweeps laterally to pass through the transverse foramen of C1 (atlas). From here, it passes around the posterior border of the lateral mass of C1 and if there is an arcuate foramen, it will pass through, then below the inferior border of the posterior atlanto-posterior atlantooccipital membrane lateral to the cervico-medullary junction. Passing superomedially, it pierces the dura and arachnoid to continue as V4.
V4 ascends anterior to the roots of the hypoglossal nerve (CN-XII) and joins its contralateral counterpart at the lower border of the pons to form the basilar artery.
Click here for more information about Deborah Pate, DC, DACBR.





