The underlying causes of knee pain and dysfunction are rarely isolated to the knee. The knee is a relatively stable joint with limited intrinsic ability to adapt to aberrant motion.
In our last article, we shared how the gluteal muscles contribute to hip extension and the transference of motion and power to the leg through the knee in a sagittal (flexion / extension motion) plane. In this installment, let's discuss how the gluteus maximus (GM) muscle also affects the transverse (internal and external rotational) planes of motion of the lower extremities.
Keep in mind that although we are emphasizing the gluteal muscles and knee, it is our intent to convey the overall interconnectedness of the body. The lower extremity is an aggregate of many structures that work together to produce locomotion.
Anatomy and Function of the Gluteus Maximus
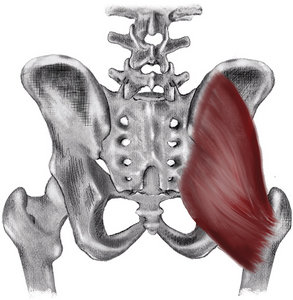 Figure 1: Schematic of the gluteus maximus. The medial-to-lateral and obliquely superior-to-inferior orientation of the gluteus maximus results in this muscle extending and externally rotating the hip.
The gluteus maximus muscle originates medially from the posterior ilium along the gluteal line and the posterior third of the iliac crest, the sacrum, the sacrotuberous ligament and the coccyx. (Figure 1) One quarter of it inserts into the gluteal tuberosity of the femur, and the remaining three quarters into the iliotibial band (which inserts into the anterior portion of the lateral condyle of the tibia at Gerdy's tubercle).
Figure 1: Schematic of the gluteus maximus. The medial-to-lateral and obliquely superior-to-inferior orientation of the gluteus maximus results in this muscle extending and externally rotating the hip.
The gluteus maximus muscle originates medially from the posterior ilium along the gluteal line and the posterior third of the iliac crest, the sacrum, the sacrotuberous ligament and the coccyx. (Figure 1) One quarter of it inserts into the gluteal tuberosity of the femur, and the remaining three quarters into the iliotibial band (which inserts into the anterior portion of the lateral condyle of the tibia at Gerdy's tubercle).
The action / function of the GM is to extend and externally rotate the hip. The GM also assists in maintaining the knee in extension due to its connection to the anterior portion of the tibia via the iliotibial band.
Weak Gluteus Maximus Muscles and Genu Valgus
Since the primary function of the GM is to externally rotate and extend the knee, a weak or inhibited GM can result in internal rotation of the femur, placing the knee into genu valgus. (Figure 2) This genu valgus position greatly increases the likelihood of an anterior cruciate ligament (ACL) injury.
When athletes fatigue, their gait degrades. If you watch an endurance runner at the beginning of a long race, their gait usually will look better than at the end of the race. This concept can also be applied to other sports and activities. As the muscles fatigue, both the gait and general athletic performance degrade.1-4
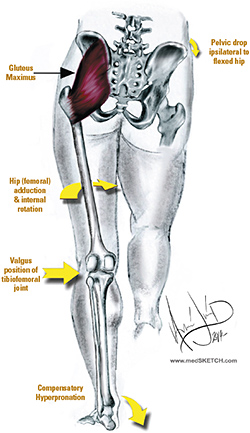 Figure 2: Gluteus maximus weakness creates a cascade of events that increases the likelihood of injury. GM weakness causes a contralateral pelvic lowering, ipsilateral internal rotation of the femur, which results in a valgus position of the knee and compensatory hyperpronation.
In regard to the GM, as the athlete fatigues, the knee is more likely to internally rotate. This shift creates the appearance of genu valgus and increases the likelihood of injury, particularly ACL injury. Fatigued athletes are more likely to injure their knees than fresh athletes.5
Figure 2: Gluteus maximus weakness creates a cascade of events that increases the likelihood of injury. GM weakness causes a contralateral pelvic lowering, ipsilateral internal rotation of the femur, which results in a valgus position of the knee and compensatory hyperpronation.
In regard to the GM, as the athlete fatigues, the knee is more likely to internally rotate. This shift creates the appearance of genu valgus and increases the likelihood of injury, particularly ACL injury. Fatigued athletes are more likely to injure their knees than fresh athletes.5
Multiple elements contribute to the degradation of athletic form resulting from fatigue. Not only does local muscle fatigue contribute to increased risk of injury, but also metabolic fatigue, aerobic fatigue, and fatigue of the central and peripheral nervous systems.6
Fatigue has been cited in contributing to or causing a lag in neuromuscular activation,7 reduced coordination,8 diminished balance9 and impeded muscle force.10-11 Studies have also shown increased electromyography (EMG) activity of the quadriceps and hamstrings as the GM fatigues.12 As a result, optimal performance patterns are substituted with suboptimal motion patterns that are more likely to contribute to injury.
Conditioning for strength and endurance is important to athletes, but so is managing rest and play time. Weekend-long tournaments, in which athletes play one game after another, will yield high rates of ACL injuries as fatigue takes its toll. Coaches must rotate players in and out of games to ensure athletic fatigue does not contribute to injury.
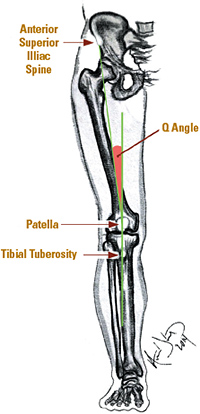 Figure 3: The Q angle (quadriceps angle) is the angle formed by the intersection of two lines: the line from the middle of the patella to the anterior superior iliac spine (ASIS) and a line from the tibial tubercle through the middle of the tubercle.
Special Considerations: The Female Athlete
Figure 3: The Q angle (quadriceps angle) is the angle formed by the intersection of two lines: the line from the middle of the patella to the anterior superior iliac spine (ASIS) and a line from the tibial tubercle through the middle of the tubercle.
Special Considerations: The Female Athlete
Women are much more prone to knee injuries than men. In fact, depending on the research, women athletes are two to nine times more likely to have an ACL rupture than their male counterparts.13 The real questions are why and what we do about it.
There has been much written about this subject, and there are several theories, but no one reason has been able to fully explain this phenomenon. Some of the possible causes include the wider Q angle (between the pelvis and the femur) found in women due to the fact that they have a wider pelvis. (Figure 3) Other factors unique to women are increased laxity of ligaments, slower reflex time, weaker hamstrings (in relationship to the quadriceps), hormonal effects of estrogen on the strength of the ACL, smaller ACL and intercondylar notch, and poor landing technique when leaping.
Determining If a Patient Has GM Weakness and/or Inhibition
One factor that can be easily identified and managed is GM weakness. Identifying gluteal weakness requires developing a keen eye for internal knee rotation and the appearance of a valgus migration during functional motion. Manual muscle testing may be used to grade more overt weakness, but gait analysis and observation of the patient moving through more functional motor patterns are better methods for identifying more subtle gluteal weakness patterns.
Observing a patient perform single-leg squats can reveal the subtle signs of a weak GM. (Figure 4) The weight-bearing leg should remain stable and straight as the patient descends. If the knee migrates medially into a valgus position, this is an indication of GM weakness. A variation of this test is to observe the patient descending stairs, again observing for medial migration of the knee.
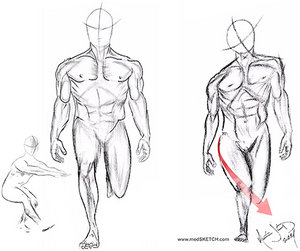 Figure 4: Testing for gluteus maximus weakness. Clinical testing of the GM can be done by having the patient perform a one-leg squat or hop or by watching the patient descend stairs. The knee should track down straight in alignment with the tibia and femur (left image). If the knee migrates medially (right image), it indicates a motion pattern fault and likely a weak gluteus maximus.
A more rigorous evaluation intended for athletes may include squat jumping (repeated jumping and landing into a deep squat). If the knees approximate, it is indicative of weak GM. Some doctors will even analyze the patient while performing single-leg hops or box jumping.
Figure 4: Testing for gluteus maximus weakness. Clinical testing of the GM can be done by having the patient perform a one-leg squat or hop or by watching the patient descend stairs. The knee should track down straight in alignment with the tibia and femur (left image). If the knee migrates medially (right image), it indicates a motion pattern fault and likely a weak gluteus maximus.
A more rigorous evaluation intended for athletes may include squat jumping (repeated jumping and landing into a deep squat). If the knees approximate, it is indicative of weak GM. Some doctors will even analyze the patient while performing single-leg hops or box jumping.
The use of video recording with performance-analysis software can aid the doctor in analyzing these motion patterns. If the athlete lands or jumps with valgus migration of the knees, the athlete should be coached in motion patterns that avoid genu valgus and internal hip rotation. They should also be instructed in a specific program of GM strengthening.
The advent of coaching, sports performance and analysis software, and mobile device applications has made it easy to record video of functional motions such as running, descending stairs, jumping and squatting. Using frame-by-frame playback to look for medial migration of the knee allows a clear view into a patient's motion patterns.
Many of these video applications come with line-drawing-analysis tools. This technology allows for video to be taken on the sports field or other locations and sent to doctors for analysis.
| Clinical Insight: Knee Manipulation
Complex joints like the knee should not be manipulated with high-velocity, low-amplitude (thrusting) manipulations injudiciously. Just because we can manipulate, does not mean we should manipulate. Clinically, we have found that when a patient says it feels like their knee needs to pop and asks for an adjustment, there is often joint effusion within the knee and it is likely to have an internal derangement, like a medial meniscus tear. This is a time to avoid thrusting manipulations of a joint. Much of the time, knee dysfunction arises from the hips and pelvis, or the foot and ankle. We are much more likely to address the foot, ankle, hip and lumbopelvic regions than the knee when treating knee impairments. Likewise, we are likely to include active care that addresses the gluteal muscles and closed-chain exercises, rather than isolating the knee with open-chain exercises like the leg extension. Frequently, we look to activate and strengthen the gluteal muscles to reduce unhealthy motion patterns and stresses from the knee. |
Determining appropriate management of a patient with GM weakness is dependent upon how far along the patient is in their rehabilitation. An athlete with no overt injury wishing to increase athletic power will start at a higher level of training than a patient recovering from injury. Nonetheless, when considering an athlete, we need to prepare for the higher rate of knee injury that accompanies fatigue and weakness by conditioning the GM for endurance and strength.
For athletes who are intent on improving performance versus rehabilitating from a state of infirmity, we like to include weighted squats with elastic-band tubing around the distal thigh, just above the knee. This provides a gentle stimulus and tactile cue that helps them to activate their GM during this motion. Other exercises that may enhance GM activation include hip thrusters from a supine bridge, lunges, kettlebell swings and squats, and box jumping.
A less intense method of exercise would use exercise tubing around the legs, just above the knees, and exercising in a partial squat with the GM activated by abduction and mild external rotation. Additionally, "monster" walks, side walking, partial squats, and hip thrusts will stimulate and strengthen the GM. Patients unable to tolerate these exercises may begin with side-lying "clams" and progress through the track.
In addition to conditioning the GM with the intent to increase strength and endurance, aberrant motion patterns should be corrected with technical motion training. This would involve training patients how to properly squat, how to activate the GM while descending stairs, and how to perform other activities of daily living. For athletes, this would include coaching in running, jumping and agility components of their particular sport. A strong GM plays a protective role in the knee and will increase power in both athletes and the general population.
Resources
- McLean SG, Felin RE, Suedekum N, et al. Impact of fatigue on gender-based high-risk landing strategies. Med Sci Sports Exerc, 2007;39:502-514.
- Gabbett TJ. Incidence of injury in amateur rugby league sevens. Br J Sports Med, 2002;36:23-26.
- Rahnama N, Reilly T, Lees A. Injury risk associated with playing actions during competitive soccer. Br J Sports Med, 2002;36:354–359.
- Murtaugh K. Injury patterns among female field hockey players. Med Sci Sports Exerc, 2001;33:201-207.
- Ortiz A, Olson SL, et al. Fatigue effects on knee joint stability during two jump tasks in women. J Strength Cond Res, Apr 2010;24(4):1019-1027.
- Kent-Braun JA. Central and peripheral contributions to muscle fatigue in humans during sustained maximal effort. Eur J Appl Physiol Occup Physiol, 1999;80:57-63.
- Chappell JD, Herman DC, Knight BS, et al. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med, 2005;33:1022-1029.
- Coventry E, O'Connor KM, Hart BA, et al. The effect of lower extremity fatigue on shock attenuation during single-leg landing. Clin Biomech, 2006;21:1090-1097.
- Greig M, Wlker-Johnson C. The influence of soccer-specific fatigue on functional stability. Phys Ther in Sport, 2007;8:185-190.
- Rodacki AL, Fowler NE, Bennett SJ. Vertical jump coordination: fatigue effects. Med Sci Sports Exerc, 2002;34:105-116.
- Ronglan L, Raastad T, Borgesen A. Neuromuscular fatigue and recovery in elite female handball players. Scand J Med Sci Sports, 2005;16:267-273.
- Orishimo KF, Kremenic IJ. Effect of fatigue on single-leg hop landing biomechanics. J Appl Biomech, 2006;22:245-254.
- Prodromos CC, Han Y, Rogowski J, et al. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy, 2007;23(12):1320-1325.
Editor's note: This article is a continuation of the discussion of the knee that began in the June 15 issue with "The Amazing Four-Bar Mechanism," and part of an ongoing series on chiropractic management of lower extremity conditions.
Dr. William Morgan, is the president of Parker University. He previously served as the White House chiropractor (2007-2016), and as the chiropractor to the United States Congress and Supreme Court (2000-2016). He was credentialed at Bethesda Naval and Walter Reed military hospitals, and was team chiropractor for the U.S. Naval Academy football team.
Dr. Amin Javid attended the University of California, San Diego, and then earned his doctorate in chiropractic medicine. He currently works with leading figures in health care and biomechanical research, and is a medical illustrator for various physicians and organizations worldwide. Contact him through his website or directly via email at
.




