Low back pain involving an apex posterior sacrum (+θX-axis misalignment) typically presents with signs of lumbosacral joint impingement or facet syndrome. The patient usually can identify the source of the worst pain by pointing to the level and side of facet involvement.
Physical / Orthopedic Findings
Several physical, orthopedic and exam findings are consistent with an apex posterior sacrum. Motion palpation reveals fixation at the lumbosacral junction, especially on extension. Fixation at the L5/S1 facet joint is most often unilateral, but bilateral fixation may be encountered. Static palpation demonstrates point tenderness, especially over the L5 spinous and the inferior articular processes of L5. The lumbosacral may show moderate edematous and sudoriferous changes.1
 FIG 1 Sacral Compression Test
Minor's sign will likely be observed when the patient rises from a chair or bench. The patient also may stand or walk in antalgic flexion or tuck the buttocks under to relieve lumbosacral impingement. Kemp's test is almost always positive for facet syndrome, especially with unilateral impingement. Note: Kemp's test should be administered with the patient standing to be as specific as possible.
FIG 1 Sacral Compression Test
Minor's sign will likely be observed when the patient rises from a chair or bench. The patient also may stand or walk in antalgic flexion or tuck the buttocks under to relieve lumbosacral impingement. Kemp's test is almost always positive for facet syndrome, especially with unilateral impingement. Note: Kemp's test should be administered with the patient standing to be as specific as possible.
Two tests, the sacral compression test and the sacral distraction test, are probably the most definitive physical or palpatory assessments for an apex posterior sacrum. (We have described these tests in detail in previous articles; see Figures 1 and 2 in this article.) In the case of an apex posterior sacrum, the sacral compression test exacerbates symptoms by narrowing the gap between the L5 and S1 articular facets; the sacral distraction test relieves symptoms by opening the joint interval at L5 and S1, and relieving tension in the capsular ligaments and periarticular soft tissues.
 FIG 2 Sacral Distraction Test
Radiographic analysis also may be used to confirm an apex posterior sacrum. The lateral lumbar view reveals the following:1
FIG 2 Sacral Distraction Test
Radiographic analysis also may be used to confirm an apex posterior sacrum. The lateral lumbar view reveals the following:1
- An increased sacral base angle greater than 45 degrees
- Hyperlordosis of the lumbar spine
- Anteriority of the gravitational stress line projected inferiorly from the center of the L3 body relative to the anterior tip of the sacrum (S1)
- Extension malposition of L5 relative to the sacral base
Radiographic Findings
Be alert to three radiographic findings that suggest instability predisposing the patient to severe facet syndrome. First is asymmetrical convergence of Van Akkerveeken's lines – projected from the inferior plate line of L5 and the sacral base. Asymmetry is indicated when the posterior, inferior tip of L5 projects past the posterior, superior tip of S1. If the AC interval (Figure 3) is four or more millimeters longer than the AB interval, hyperextension misalignment of L5 on sacrum is indicated.3-4
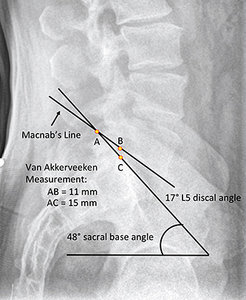 FIG 3 Lateral Lumbar Radiograph
The second finding is increased discal angle at the lumbosacral junction, as revealed by Macnab's lines. As Cox observes, an angle formed by the inferior plate line of L5 and sacral base that exceeds 15 degrees is a sign of severe facet syndrome "due to hyperextension of the superior segment on the lower motor unit."3
FIG 3 Lateral Lumbar Radiograph
The second finding is increased discal angle at the lumbosacral junction, as revealed by Macnab's lines. As Cox observes, an angle formed by the inferior plate line of L5 and sacral base that exceeds 15 degrees is a sign of severe facet syndrome "due to hyperextension of the superior segment on the lower motor unit."3
The third radiographic finding is hyperextension subluxation of L5 on the sacrum. Cox observes that if the superior facet of S1 telescopes above the superior line of Macnab (inferior plate line of L5), "facet imbrication"2-3 is indicated. The result is vertical stenosis of the intervertebral foramen at L5-S1.
Adjusting the Problem
To adjust a posterior sacral apex, assume a straightaway stance on either side of the patient. Using the inferior contact hand, take a contact with the heel of the hand on the third sacral tubercle. Take a superior-to-inferior (S-I) tissue pull to take out soft-tissue slack. Extend the wrist of the contact hand slightly to preload for the thrust.
 FIG 4 Apex Posterior Sacrum Adjustment
Position the bony pisiform of the superior, stabilization hand in the anatomical snuff box of the contact hand and wrap the fingers around the wrist. Apply an arcing thrust directed toward the sacral apex. The line of correction is superior-to-inferior (S-I) and posterior-to-anterior (P-A.)3,5
FIG 4 Apex Posterior Sacrum Adjustment
Position the bony pisiform of the superior, stabilization hand in the anatomical snuff box of the contact hand and wrap the fingers around the wrist. Apply an arcing thrust directed toward the sacral apex. The line of correction is superior-to-inferior (S-I) and posterior-to-anterior (P-A.)3,5
Immediate post-checks may not be especially useful, since the complaint frequently involves some local swelling and edema; as well as muscle hypertonicity and point tenderness at the lumbosacral junction, especially with acute onset of symptoms. Even after a successful adjustment, symptoms may persist for several hours. Therefore, it would be prudent to advise the patient to avoid strenuous activity and lifting for the rest of the day. The ideal time to re-evaluate the complaint is at the patient's next visit.
References
- Pettersson HA, Green, JR. How to Find a Subluxation. Davenport, IA: Black Athena Press, 2003.
- Macnab I. Backache. Baltimore: Williams & Wilkins, 1977.
- Cox JM. Low Back Pain: Mechanism, Diagnosis and Treatment, 7th Edition. Lippincott, Williams & Wilkins, 2011.
- Van Akkerveeken P, O'Brien J, Park W. Experimentally induced hypermobility in the lumbar spine. Spine, 1979;4(3):236-241.
- Pettersson HA. Pelvic Drop Table Adjusting Technique. Davenport, IA, 1999.
Dr. Howard Pettersson, a 1976 graduate of Logan College of Chiropractic, is an associate professor of technique at Palmer College of Chiropractic. He was the senior editor of Activator Methods Chiropractic Technique – College Edition, published in 1989, and published Pelvic Drop Table Adjusting Technique in 1999. His most recent publication, written with Dr. Green, is How to Find a Subluxation, published in 2003.
Dr. J.R. Green is a 1988 Graduate of Palmer College of Chiropractic. He retired from the Palmer faculty after many years of teaching basic sciences and chiropractic technique. He is currently in private practice in Galva, Ill., and is also an adjunct professor of chemistry with the Eastern Iowa Community College District. Dr. Green was one of the writers of Activator Methods Chiropractic Technique (1997) and also worked as a technical writing consultant on Activator Methods Chiropractic Technique – College Edition and Pelvic Drop Table Adjusting Technique.




