New-patient consult: a 52-year-old man with a four-year history of low back pain exacerbated by walking. Patient states that in the past year, he experiences pain into his buttocks and legs when walking.
His initial neurologic and orthopedic exams are unremarkable. Lumbar spine study demonstrates degenerative changes at the L4-5 and L5-S1 levels, with the L5-S1 level most remarkable.
Missing Something?
Do you notice the changes in the L3 vertebral body? (Fig.1) Even with my many years of reviewing spine films, I might have ignored the changes and focused on the clinical symptoms, leading me to just correlate the degenerative changes at the L5-S1 level.
Should you evaluate this patient further? The patient's clinical symptoms and plain films seem to correlate with the degenerative disc disease at the L5-S1 level. But his symptoms are not improving with treatment. The next step would be to refer the patient for an MRI to evaluate neurological impingement from the disc disease and determine what's happening at the L3 vertebral body.
Sagittal MR slice demonstrates the degenerative disc disease and disc herniation at the L4-5 and L5-S1 levels; and also indicates the L3 vertebral body is not normal. (Fig. 2) There are many reasons for changes demonstrated in the vertebral body: osteoblastic metastases, prostate cancer, lymphoma, Paget's disease, tuberculous spondylitis and hemangioma being the most probable differential diagnoses.
The patient does not have a history of prostate cancer and is otherwise healthy. To determine the cause of the changes demonstrated at the L3 vertebral body, we need further laboratory tests and possibly a bone scan. Laboratory tests should include alkaline phosphatase, calcium and maybe a PSA level.
Paget's Disease
The patient's alkaline phosphatase level is 350 (reference range 40-125). Bone scan demonstrates increased uptakes at the L3 vertebra. Both of these findings are indicative of Paget's disease. (Fig. 3)
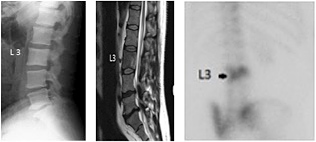 Clockwise from left: FIG 1 Lumbar spine; note changes in L3 vertebral body. FIG 2 Sagittal MRI lumbar T2 weighted image confirming changes at L3. FIG 3 Bone scan showing increased uptakes at L3 indicative of Paget's disease.
Typically, patients with Paget's disease present with an isolated elevation in alkaline phosphatase level, but otherwise normal results of biochemical testing. In fact, the first indication of Paget's disease of bone is often an elevated serum alkaline phosphatase level or an abnormal radiograph in a patient whose health is being investigated for other reasons.1
Clockwise from left: FIG 1 Lumbar spine; note changes in L3 vertebral body. FIG 2 Sagittal MRI lumbar T2 weighted image confirming changes at L3. FIG 3 Bone scan showing increased uptakes at L3 indicative of Paget's disease.
Typically, patients with Paget's disease present with an isolated elevation in alkaline phosphatase level, but otherwise normal results of biochemical testing. In fact, the first indication of Paget's disease of bone is often an elevated serum alkaline phosphatase level or an abnormal radiograph in a patient whose health is being investigated for other reasons.1
Paget's disease is associated with abnormal bone turnover that in turn, is due to an imbalance between osteoclastic and osteoblastic activity; an increase in osteoclast numbers and activity; and often affects multiple sites throughout the skeleton. Increased bone resorption is then compensated by an increase in bone formation.
Due to the accelerated bone turnover, new collagen fibers are not laid down in an orderly, linear fashion, but rather in a disorganized manner. The resultant bone is a mosaic of woven and lamellar bone that is mechanically insufficient and at increased risk for fracture or deformity.
Infection has been postulated as a potential trigger because viral inclusions within the nuclei of osteoclasts from patients with Paget's disease have been found which resemble the paramyxovirus class that includes measles, respiratory syncytial and canine distemper viruses.
There is also a genetic predisposition to this disease, but recent data indicates the incidence and severity of Paget's disease of bone is decreasing; possibly reflecting the changes in environment that may mitigate the predisposition.2
The Disease Process
In general, there are three phases to the disease process. The lytic phase occurs first, when osteoclastic activity is the greatest. In this phase, the radiographic appearance can mimic osteoporosis; however, the osteopenia is localized.
The second phase is described as a mixed phase, which has features of both osteoblastic and osteoclastic activity. In this phase, trabecular and cortical thickening with enlargement of the bone can be seen.
The third phase is blastic, with osteoblastic activity predominating, giving the typical appearance of sclerosis with disorganized trabecular patterns. (I would like to suggest there is also a fourth, final phase when the process of bone turnover seems to stop or burn itself out. On bone scans, the lesions no longer demonstrate an increased uptake, but the bone still appears abnormal on X-ray.)
Imaging Findings
In the lytic phase, well-defined osteolytic lesions can be seen in the skull, known as osteolysis circumscripta. Lytic lesions in the long bones have more of a wedge shape with sharp, lucent leading edges where the bone resorption is occurring. The mixed phase demonstrates coarsening and thickening of the trabecular pattern and cortex along lines of stress, as well as disorganized areas. In the spine, cortical thickening can result in the picture-frame appearance of the vertebral body.
In the blastic phase, areas of previous trabecular and cortical thickening is often obscured by extensive sclerosis, as in the vertebrae with the "ivory vertebral body." Bone enlargement can also be seen in this phase. In the skull, scattered areas of focal sclerosis, "cotton wool," can be seen.
The CT appearance is very similar to plain radiographic findings; however, since the neural arches of the vertebrae are particularly difficult to assess on radiographs, CT is best for examining the neural canal and foramina for impingement due to the enlargement of bone.
MRI appearance is not particularly specific for Paget's disease, but it is sensitive. The trabecular and cortical thickening demonstrates a low signal on all pulse sequences. Heterogeneous bone marrow T1 and T2 signal can be seen in both the lytic and mixed phases, especially in water-sensitive images. In the late blastic phase, there is a low signal throughout the marrow due to the sclerosis.
Nuclear medicine scans can show the extent of the disease in the skeleton, even before there is an abnormality on the radiographs. The amount of uptake to a specific area depends on the blood flow and the amount of new bone formation. Very late in the disease process, the bone scan may appear normal even with continued abnormalities on radiographs.
Clinical Ambiguity?
Initially, there do not appear to be any significant symptoms. The disease often is discovered as an incidental finding on X-ray. The most common symptom patients complain of is deep bone pain localized to the area of active disease. Along with local pain, there is tenderness and increased warmth.
Bone enlargement can cause neuromuscular symptoms, as in spinal stenosis; and deafness from skull involvement. Patient may also suffer from bowing deformities, decreased range of motion and kyphosis. Complications most commonly occur form osseous weakening with fractures and bone deformity; as well as secondary osteoarthritis from altered biomechanics. Osteosarcoma is rare, occurring in less than 5 percent of cases.2
In the case I present here, the patient was not aware of any symptoms associated with the changes involving the L3 vertebral body. It remains to be seen if this disease process will ultimately affect the patient's spinal canal.
When there are symptoms of bone pain, often it can be controlled by aspirin or other analgesics. Use of parathyroid hormone (PTH) antagonists, such as calcitonin and bisphosphonates, can reduce bone turnover and improve the biochemical abnormalities.4 Of course, I would refer symptomatic patients to a specialist in the field.
References
- Alikhan MM, et al. Paget Disease. Medscape.com, updated Nov. 21, 2016.
- Daphne J Theodorou DJ, et al. Imaging of Paget disease of bone and its musculoskeletal complications: review. Am J Roentgenology, 2014 Oct;96(6 supplement).
- Dell'Atti C, et al. The spine in Paget's disease, Skeletal Radiol, 2007;36(7):609.
- Sabharwal R, et al. An insight into Paget's disease of bone. Nigerian J Surg, 2014;20(1):9-15.
Resources
- Information for Patients About Paget's Disease of Bone. NIH Osteoporosis and Related Bone Diseases National Resource Center.
- Rodan GA, et al. Therapeutic approaches to bone diseases. Science, 2000 Sep 1;289(5484).
Click here for more information about Deborah Pate, DC, DACBR.





