Axler and McGill have demonstrated that muscle output as a percentage of maximum voluntary contraction ability (MVC) and spinal load as a measure of spinal compression and shear forces can be measured for a variety of exercises.1 Ideal exercises are those that have a high muscle challenge to spinal load ratio. Janda has presented a model for rehabilitation which emphasizes that the quality of the movement is more important than the strength.2 For example, an individual may have excellent strength in performing leg raises, but if they overactivate the synergist hamstring or erector spinae muscles for the agonist gluteus maximus, lumbar overstrain will occur.
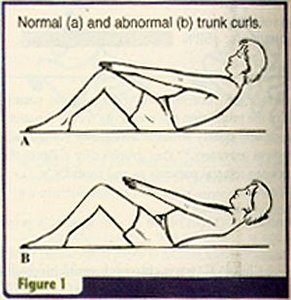
To learn to isolate target muscles while minimizing joint overstrain, a systematic approach has been recommended. If movement patterns have been identified where muscle imbalance is present -- for instance, excessive iliopsoas activity during trunk curls -- then relaxation of the overactive muscle should generally precede any strengthening exercise. Naturally, if an overactive muscle is not relaxed prior to a strengthening exercise, the result will be reinforcement of the muscle imbalance.
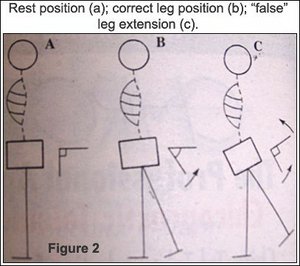
The consequence of muscle imbalance and faulty movement patterns is joint overstrain. Think of an individual performing leg extensions with a shortened iliopsoas. They will have hypomobility in their hip joint in extension and the movement will automatically follow the path of least resistance and occur around an axis of the lumbosacral joint. Repetitive overstrain will be the inevitable result.
Practice Tip
When a patient reports pain, always evaluate for a related muscle imbalance and a faulty movement pattern.
Evaluate if the pain is coming from the overstrained area and if there is a related hypomobile joint that is functionally linked.
Example:
Chief complaint: low-back pain
Activity intolerance: walking, standing
Examination findings:
- increased lumbar lordosis during prone hip extension (see Figure 2);
- hypomobile hip joint in extension;
- muscle imbalance -- tense iliopsoas and inhibited gluteus maximus.
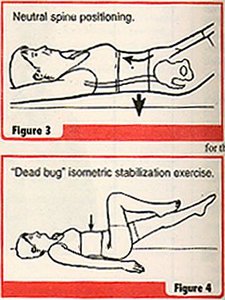
Once the overactive muscle is relaxed, safe back training follows three basic steps (see Table I below).3 First, train the individual how to produce spinal/pelvic joint motions through a full range, and how to find their "neutral spine/pelvis position." Second, train the individual to maintain the "neutral joint position" of the spine/pelvis while load is added distally through the arms and/or legs. This motor control is isometric stabilization. Third, train the individual to control the "neutral joint position" of the spine/pelvis during trunk movements. This is called dynamic stabilization. Unfortunately, this training requires some cortical effort. However, the benefit is that once it is trained, a new motor program will form that will subcortically protect vulnerable joints from injury on a reflex, semi-automatic basis. To facilitate the formation of a new motor program, labile surfaces (balls, foam, platforms) are used as much as possible. By challenging balance, afferent pathways are spontaneously facilitated in a concentrated way.
Table I: Safe Back Training Steps
1. Relax overactive antagonist or synergist muscles
2. Train awareness of spinal/pelvic position (Level 1 -- see Figure 3)
3. Train isometric stabilization with distal loading (Level 2 -- see Figure 4)
4. Train dynamic stabilization with trunk loading (Level 3 -- see Figure 5)
Note: Utilize labile training devices whenever feasible.
These safe back principles have been incorporated into remobilization workouts for acute patients, reactivation workouts for subacute patients, flexibility workouts for recurrent patients or prevention, and gym ball workouts for recurrent patients or prevention.4,5,6,7,8,9,10 Exercise is a powerful tool in teaching patients to develop an internal locus of control for managing their pain. Educational material warning against the dangers of prolonged bed rest and the benefits of activity are essential.8,11 Consensus-based low back guidelines emphasize that active care or exercise be incorporated no later than the end of the first month of care.12 Recent evidence suggests that specific exercises utilizing the above safe back principles are a key to achieving successful outcomes even with chronic patients.13
References
1. Axler CT, McGill SM. Low back loads over a variety of abdominal exercises: searching for the safest abdominal challenge. Med Sci Sports Exerc 1997;29:804-810.
2. Janda V. In: Liebenson C (ed.) Rehabilitation of the Spine: A Practitioner's Manual. Williams & Wilkins, Baltimore, 1995.
3. Grant G, Jull G, Spencer T. Active stabilization training for screen-based keyboard operators: a single case study. Aus J Phy Ther 1997;43:235-242.
4. Liebenson C, Chapman, DeFranca C. Safe Back Workout: Reactivation and Remobilization: Beginner Level. Williams & Wilkins, Baltimore, 1998.
5. Liebenson C, Perri M, Murphy D, DeFranca C. Safe Back Workout: Flexibility, Breathing and Relaxation Routine. Williams & Wilkins, Baltimore, 1998.
6. Liebenson C, DeFranca C, Gluck N. Safe Back Workout: Low Back and Abdominals and Low Back: Advanced Level. Williams & Wilkins, Baltimore, 1998.
7. Liebenson C, DeFranca C, Gluck N. Safe Back Workout: Glutes and Thighs: Advanced Level. Williams & Wilkins, Baltimore, 1998.
8. Liebenson C, Oslance J. 20 minute exerball workout. The Gym Ball Store, San Diego, 1997. (800) 393-7255.
9. Oslance J, Liebenson C. The proprio system. The Gym Ball Store, San Diego, 1996. (800) 393-7255.
10. Murphy D, Liebenson C, Ierna G, Gluck N. Lumbar Spinal Stabilization: Floor Exercises. ACES, Wading River, New York, 1998.
11. The Back Book. ISBN 011-702078-8. The Stationary Office, 011-44-17-1873-9090.
12. Bigos S, Bowyer O, Braen G, et al. Acute Low Back Problems in Adults. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, 1994.
13. O'Sullivan P, Twomey L, Allison G. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine 1997;24:2959-2967.
Craig Liebenson, DC
Los Angeles, California
cldc-flash.net
Click here for previous articles by Craig Liebenson, DC.





