In the June issue, I discussed why it was important to begin to do impairment ratings. Now, let's look at how to deliver an effective radiology-based impairment rating report using the AMA Guides, 5th or 6th edition (The Guides). Key areas of The Guides for which DCs have special emphasis include spinal impairment of the various regions: cervical, thoracic and lumbar spines, as well as the pelvis. The focus here is on the section with the spinal impairment chapters for the regions of the spine. The Guides describe in detail AOMSI – alteration of motion segment integrity.
Determining AOMSI: Translational vs. Angular
This AOMSI radiographic finding is only accepted by The Guides to be visualized on plain-film lateral flexion and extension views, also known as motion studies. Let's address the cervical spine as an example. You do not use MRI or CT for determining AOMSI. The measurement is determined by assessing how one vertebra slips forward or backward on top of another vertebra, as measured on the lateral flexion and extension views.
The measurement is obtained by placing points/dots as shown on the diagram and determining how many millimeters the anterolisthesis or retrolisthesis occurs, if any. The measurement in millimeters is the amount of slippage. (Figure 3) This is known as translational AOMSI.
 FIG 1 Translation method for AOMSI determination using the AB ratio in AMA Guides, 6th Edition.
A value greater than 2.5 millimeters in the thoracic spine or greater than 4.5 millimeters in the lumbar spine, and greater than 3.5 millimeters in the cervical spine, qualifies as a loss of structural integrity. AOMSI can be either a loss of motion segment from increased translation or angular motion, or both.1
FIG 1 Translation method for AOMSI determination using the AB ratio in AMA Guides, 6th Edition.
A value greater than 2.5 millimeters in the thoracic spine or greater than 4.5 millimeters in the lumbar spine, and greater than 3.5 millimeters in the cervical spine, qualifies as a loss of structural integrity. AOMSI can be either a loss of motion segment from increased translation or angular motion, or both.1
In the 6th edition, the AOMSI measurement for the cervical spine is described as the translation measurement being greater than 20 percent anterior or greater than 20 percent posterior to the relative translation of one vertebra on another. This AB ratio measurement is shown on Figure 1.
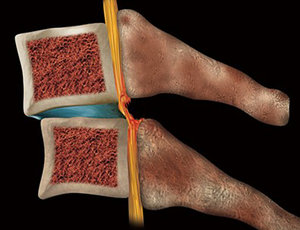 FIG 2 Anterolisthesis image indicating ligament injury.
There could also be angular AOMSI, whereby the vertebrae are tipping or angulated in a flexed or extended position by more than 11 degrees over the other adjacent vertebrae. (Figure 4) The instruction is too long for this article, but is clearly described in The Guides. A line is drawn along the posterior bodies of the vertebrae below and above the motion segment in question on dynamic flexion and extension of the lateral X-rays of the spine.
FIG 2 Anterolisthesis image indicating ligament injury.
There could also be angular AOMSI, whereby the vertebrae are tipping or angulated in a flexed or extended position by more than 11 degrees over the other adjacent vertebrae. (Figure 4) The instruction is too long for this article, but is clearly described in The Guides. A line is drawn along the posterior bodies of the vertebrae below and above the motion segment in question on dynamic flexion and extension of the lateral X-rays of the spine.
Angular motion AOMSI of more than 11 degrees greater than each adjacent level on the flexion radiograph only qualifies the individual for this ratable impairment. Alternatively, there may be complete or near-complete loss of motion of a motion segment due to developmental fusion, surgical arthrodesis, or preserved motion with disc arthroplasty.2
Which Should I Use?
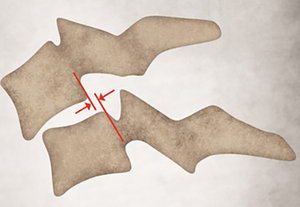 FIG 3 Translation method in AMA Guides, 5th Edition, measuring anterolisthesis.
The subtle differences between the 5th and 6th editions requires determining which one your state allows or which one you are more comfortable in measuring, if both are allowed. While this may seem complicated, it is quite simple once you invest one hour in reading The Guides' spine chapter and watching a 10-minute tutorial on how to apply the lines to perform the measurements.
FIG 3 Translation method in AMA Guides, 5th Edition, measuring anterolisthesis.
The subtle differences between the 5th and 6th editions requires determining which one your state allows or which one you are more comfortable in measuring, if both are allowed. While this may seem complicated, it is quite simple once you invest one hour in reading The Guides' spine chapter and watching a 10-minute tutorial on how to apply the lines to perform the measurements.
Advanced software with AI technology that allows the doctor to take about three minutes and place a dot on the four corners of the vertebral bodies of C3 through C7 on the lateral flexion and extension views will create the measurements automatically for either 5th or 6th edition measurements. Once you use the digital X-ray software to place those dots/points, then the calculation and measurement are performed by the software and the determination of a ratable impairment is established into a narrative radiology report.
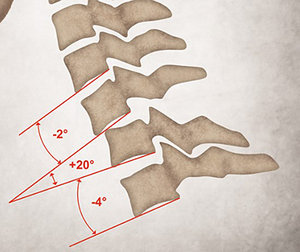 FIG 4 Angulation measurement method for AOMSI (greater than 11 degrees is ratable).
Assembling the Radiology Report
FIG 4 Angulation measurement method for AOMSI (greater than 11 degrees is ratable).
Assembling the Radiology Report
The next step is to assemble the information and the assessment into the radiology report. Clearly describing the findings of the translational or angular measurements and if they are ratable are critical to having the person reading the report be able to understand what it means. A chart or grid listing if the various segmental levels are normal, abnormal or ratable helps the reader get an easy understanding.
Using colors such as red to designate something abnormal helps visualize something is wrong with the patient and that the measurement is important to note. Having schematic diagrams or graphics to demonstrate how the measurement was obtained, or how the ligament can be injured in a retrolisthesis or anterolisthesis measurement, is helpful in some cases. Plus, including into the body of the report an image of the actual flexion / extension X-rays with line drawings being demonstrated and the measurement annotated add to the visual impact of evidence.
Additional Considerations
When you get to the radiology report impressions and conclusions section, you will need to select a number; a single number, not a range, based on the respective 5th or 6th edition AMA Guides to apply a rating. For the sake of this article, there is a lot more that goes into a whole-person impairment (WPI) if you are assessing other body parts and other injuries separate from the AOMSI component, but let's assume AOMSI is the only portion we are assessing and rating, which leads us to a simplified selection from the impairment tables for the various spine regions.
For example, an AOMSI of greater than 3.5 mm at one level of the cervical spine would garner an impairment rating of minimally 25 percent WPI (5th edition, page 392, Table 15-5). That rating is significant. In the 6th edition, only one vertebral motor unit level of AOMSI equates to an impairment of somewhere between 4 percent and 14 percent, depending on radiculopathy findings and other history, examination and clinical testing results. If it were two or more segmental levels of AOMSI, it would elevate to 15-30 percent depending on clinical radiculopathy and other findings (6th edition, page 564, table 17-2.)
You cannot give a range of percentages for WPI; it must be a specific number within the range. The purpose of this discussion on AOMSI is not to describe the entire AMA Guides for impairment, but to show how just one section using AOMSI can be used by itself to demonstrate impairment.
Using references of published literature papers in your report is valuable in adding further credibility. You have relied on The Guides and other peer-reviewed published literature, as well as your clinical experience and expertise combined with the patient's clinical presentation. Document the patient's agreement and desire to have you perform the impairment rating demonstrating their preference for this evaluation to be performed.
The final step after creating the professional radiology report in a format that is easily digestible and understood, is to present the report to the patient, the attorney and possibly the claim adjuster.
Practice Pearls
Being confident and authoritative is critical to your success. There is no need to be bashful about following The AMA Guides and the customized report generated with assistance from software with your personalized commentary added. Being factual and to the point in a succinct manner wins the day. That means a satisfied attorney who refers more cases to you; and a relieved patient knowing you are applying scientific, validated and standardized measurements accepted in courts across the country.
The information may seem overwhelming if you have never performed an impairment rating. I can assure you that after having testified in court on 32 personal-injury cases and over 90 depositions, it gets easier each time as long as you prepare and keep it simple. That's why a detailed radiology report allows you to explain AOMSI findings in a courtroom because the information is in your hands.
Whether you create your own or rely on a software tool to help generate the AOMSI measurements and the radiology report for you, your added customizations can provide a valuable service your patient deserves and attorneys love. If you are going to care for personal-injury cases, you owe it to them to be knowledgeable on impairment ratings or have a referral relationship with a chiropractic colleague who will provide the service. DC's are the perfect spinal health care experts to deliver this service.
References
- The AMA Guides, 5th Edition: p. 378.
- The AMA Guides, 6th Edition: p. 578.
Click here for previous articles by Steven Kraus, DC, DIBCN, CCSP, FASA, FICC.





