The Medical Students
Fourth-year medical students from the University of Chicago were presented with a standardized whiplash patient to test their clinical perspicacity. He was a 21-year-old male who gave a history of being a passenger in a car that was struck from the rear at a speed of 25 mph. Shortly after the crash, he began to experience neck pain and was transported by ambulance to the ER. Students were asked whether they would order radiographs of his neck, and for their level of confidence in their decision. They were then presented with a variable of the abstract from a recent paper by Stiell, et al.,2 in which the authors developed a radiography algorithm. (I will discuss that paper next.)
After reviewing the abstract, the students were allowed to reaffirm their decision to order plain films, or to change it, and were asked to once again rank their level of confidence. Most of the 165 students did endorse the idea of ordering radiographs initially. Many apparently changed their minds after being exposed to the abstract informing them that radiographs were unnecessary under the circumstances. Of those initially rejecting the idea of radiographs, their confidence in that decision was strengthened by the abstract.
These medical students correctly assigned the proper weight in accordance with the relative reported sensitivity vs. specificity (i.e., high sensitivity and low specificity would be preferable to low sensitivity and high specificity). However, the results showed that the students did not consider the prospective cohort design more persuasive than the weaker case review design. Of course, other factors could have influenced their decisions.
The standardized patient completed a questionnaire for each medical student, reporting the depth of the exam. Sixty-seven percent correctly inquired as to whether the patient had numbness and tingling in the upper extremities. However, only 21% palpated the posterior neck, and only 17% asked the patient to turn his head from side to side. A scant 11% did all three. This is disturbing, but perhaps not surprising, in light of another recent study, which reported a surprisingly low level of knowledge of musculoskeletal disorders among a group of medical residents.
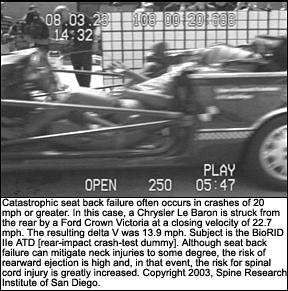
One wonders what might be the basis for the seemingly absurd recommendation to forego radiographs in a 25 mph rear-impact motor vehicle crash. Carle Ward has reported that spinal fractures, dislocations, and spinal cord injuries are not uncommon in rear-impact crashes in which delta Vs are often only in the 15-20 mph range,3 as represented below.
While at least one study has shown that police officers are able to gauge collision velocity from damage severity with some accuracy, my experience is that real-world subjects nearly always overestimate crash speed. I suspect there are a number of explanations for this observation, including the volume of the resulting crash noise and the subjective violence of the collision. Patients may also be concerned that physicians will not take them seriously if the physicians perceive the crash to be trivial. Meanwhile, it is not clear from reading the present paper how the Canadian authors arrived at the 25 mph threshold for safety, or whether other occupant risk factors were considered, such as the nature of presenting symptoms, the patient's age, spinal condition, etc. However, it seems unwise to base a criteria for radiography on a crash metric that has been shown to be a) not strongly correlated with injury risk; b) unlikely to be accurately estimated by vehicle occupants; and c) only somewhat better gauged by police.
In general, the authors of this paper endorsed the Canadian guidelines and anticipated that the medical students would either forego the radiographs initially or decide against them after reviewing the abstract of the Canadian paper. Interestingly, students who were more "in tune" with the epidemiological and clinical literature, via-à-vis c-spine trauma and MVC, unequivocally chose to examine the c-spine radiographically, including the use of flexion and extension views, as recommended by some radiologists.4
The Canadian C-Spine Rule Study
So, what is this Canadian c-spine "rule" and how was this research conducted? Perhaps a better question might be, "Why should we be concerned?" The results of the study were reproduced in JAMA, one of the most influential of the American medical journals. It is likely that it will not escape the attention of those interested in medical cost containment. It could become transmogrified into public policy in Canada, in a way similar to that of the British Columbia Whiplash Initiative, which used the Quebec Task Force on Whiplash Associated Disorders' (QTF-WAD) dubious guidelines to influence medical decision-making by practitioners there. That project, of course, was put together by the Insurance Corporation of British Columbia, the chief insurer for the province. (The QTF-WAD was also financed by the insurance industry.) This c-spine rule study was funded, at least in part, by the Ontario Ministry of Health Emergency Health Services Committee. One of the authors of the present paper, incidentally, has also been active in the development of a decision rule for whiplash.5
The purpose of this project was to develop a decision rule, or algorithm, that could be reliably used by emergency room (ER) physicians to make both rational and cost-effective decisions about when to use radiography (and when not to) in instances of conscious, alert and stable patients suffering some type of blunt trauma to the head or neck. The operant definitions here are a Glasgow Coma Scale (GCS) of 15 (alert) and no major disruption of vital signs (stable).
The authors studied a consecutive series of 8,924 cervical trauma patients who were seen at 10 Canadian hospitals for acute blunt injury to the head or neck. (Those deemed to have trivial injuries, such as facial laceration, were excluded.)The binary issue to decide was whether the patients had a "clinically important c-spine injury" or a "clinically unimportant c-spine injury."
The ER physicians in the study did receive some training/briefing prior to participation, but were allowed to make their own decisions as to whether to order radiographic studies of the patients they attended. As a result, 6,145 sets of film were exposed. Most consisted of three-view studies. Additionally, some physicians elected to acquire flexion and extension views, but the number of these studies was not reported. Blinded radiologists later reviewed the radiographs and determined whether a clinically important lesion - defined as fracture, dislocation, or ligamentous instability - was present. (Note that fractures of transverse processes that did not involve a facet joint, fractures of the spinous processes not involving the lamina, compression fractures of less than 25% loss of height, and osteophyte avulsion fractures were not considered "important" for purposes of this study.
Patients who did not have radiographs taken were interviewed by telephone 14 days later. If they had a) neck pain that was more than mild; b) restriction of motion in the neck more than mild; c) the need for a cervical collar; or d) a neck injury preventing a return to usual activities, they were considered to have suffered an "important" injury. Rather remarkably, however, none in this group (n=2,779) was found to have such an injury.
The authors analyzed a number of variables from the case files, doctors' records, and the radiographs, and developed an algorithm (rule) that had 100% sensitivity and 42.5% specificity for what was deemed an important lesion. From this, it was speculated, the number of radiographic studies could have been reduced, with a corresponding large cost savings. The authors estimated that using the rule would have resulted in 58.2% of cases in the present cohort getting radiographs, vs. the actual rate of 68.9%. The "rule" is presented on page 28.
The potential problems with such an algorithm are obvious. One wonders, for example, what methods ER physicians use cto lassify rear-impact crashes in terms of crash speed. According to the algorithm, few should necessitate radiographs - yet the literature clearly shows that a significant proportion of these victims will be unstable. In fact, spinal cord injuries do occur in rear-impact crashes when the delta V is in the 15-20 mph range or higher.4
The authors also made this pronouncement: "Clinically unimportant c-spine injuries, according to the academic surgeons in our survey, require neither stabilizing treatment nor specialized follow-up, and are unlikely to be associated with long-term problems." This survey was not described in any more detail, and the opinions reflect those of spine surgeons in general, but not the epidemiological literature. As the authors pointed out, this rule will now have to be validated in a large sample of real cases of c-spine trauma. However, based on my analysis of the methodology used; the assumptions made by these authors; my clinical experience; and my familiarity with the c-spine trauma literature, I would not predict it would survive strong scientific scrutiny.
Readers should consider a few potential problems with the conclusions. First, it should be clear that the majority of the cohort did not have any follow-up. This is a critical limitation of the study and does not provide the researchers with meaningful feedback beyond the limited amount of time patients remain in the ER. Only the 2,779 patients who did not have radiographs originally taken on the day of injury were followed, and this sample is potentially skewed by the fact that they were the very ones who did not impress the ER doctors enough to order radiographs in the first place. Thus, for 69% of the cohort, comprising, potentially, the more severe cases, there was not so much as a 24-hour follow-up, much less a long-term follow-up. Moreover, the authors reported that only 1.7% of the cohort did have "clinically important" injuries. This number - in conjunction with a large body of clinical and epidemiological literature - suggests terminology may be an important issue. For example, if you have a myocardial infarction (MI) and survive, would it be a clinically unimportant MI? ER departments and the patients themselves might offer differing opinions.
From my experience working in hospital ERs and in clinical practice, and from a knowledge of the epidemiological and clinical literature, I find it more than remarkable that, out of 2,779 patients who had sufficient reason to visit the ER on the basis of some kind of injury event, not a single one had significant (i.e., more than mild) symptoms after 14 days. Consider, for example, that 67% of the 8,924 subjects in this study (5,979) were injured in MVCs. Statistically, about 60-70% of these (3,587+) would have been rear-impact crashes. The risk for injury in a rear-impact crash is known to be about 35%; however, this study, by design, selected only those who were injured.
Consider also that about 35-50% of the patients, statistically, would have symptoms well beyond 14 days (even though a delay in onset might have prevented the ER physicians from appreciating the significance of the injury initially). So, we might have expected as many as 1,200 individuals to have been sufficiently symptomatic in the follow-up group to have been rated "clinically important." Again, the literature clearly demonstrates that delayed onset after CAD injury is a common phenomenon. Thus, the potential for false negative is highest in the largest group, since any of them might have been radiographed and released after the radiologists found no fracture or dislocation.
Much of the logic and reasoning surrounding the difficult issues facing the authors here is convoluted. On the one hand, it is clear that radiographs miss not only most soft-tissue injuries to the spine, but a remarkable percentage of fractures. For example, Woodring and Lee6 showed that cross-table lateral films (commonly taken in hospital ERs) missed 67% of the fractures and 45% of the (medically-defined) subluxations in a series of 216 patients. Another recent study confirmed the profoundly low sensitivity of plain radiography in spinal trauma.7 On the other hand, the reason for the study is that it is precisely this technology that we typically turn to first in the ER. So, rational decisions still must be made concerning the use of radiology, regardless of its sensitivity in acute c-spine trauma. One wonders, however, whether the savings in radiographs would be offset by the cost of malpractice suits and other costs incurred as a result of missed/late diagnoses.
There are also definitional problems. What do the authors mean by "ligamentous instability," exactly? They are apparently confident that it can be ruled out with a three-view static radiographic series of the neck, despite the exhortations in the radiology literature that, for this, flexion and extension views are "essential."4 There is virtually no evidence that spinal stability is adequately assessed in a three-view study. So, the present study begs as many questions as it answers. Ultimately, were the authors to look at long-term follow-up and measure downstream costs, the savings in obviated radiography charges might not be justified after all. But that may be the next study.
Parting Thoughts
This is an interesting example of how medical decision-making evolves. We have just seen how medical students' decisions in an ER setting can be influenced by studies that are essentially incomplete and rife with untested and potentially incorrect premises. Incomplete, because a study lacking follow-up does not answer important questions needed to make these decisions. The problem with incorrect premises is beyond the scope of this paper, but several should be obvious already. Notwithstanding these issues, how many of those with "normal" radiographs later returned with ongoing complaints? How many fractures or ligamentous injuries were missed on the three-view series? By dint of its design, the study can't answer those very important questions. Nevertheless, the casual "read" of an abstract can be influential and have potentially far-reaching effects.
The practice of emergency medicine is, by its very nature, incomplete. Its unassailably noble purpose is to save lives or to triage sick people. It enjoys the luxury of relegating treatment of non-life-threatening conditions to other practitioners. But, while this myopic nature of emergency medicine is both necessary and acceptable, it does not necessarily apply to practitioners for whom there is a clinical tomorrow or end point in patient care - clinicians who continue the process of diagnosis and management to its logical conclusion.
Studies of this kind can have potential significance for chiropractic physicians who also require cervical spine films to rule out other contraindications for manipulation. In fact, practitioners who perform spinal manipulation nearly always have a higher "need to know" (in terms of the patient's radiographic status) than practitioners treating conditions with medication only. Thus, in my view, there is more justification than mere academic curiosity for critically evaluating this genre of research.
References
- Schwartz A. Medical students' application of published evidence: randomized trial. BMJ 2003;326 (7388):536-538.
- Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian c-spine rule for radiography in alert and stable trauma patients. JAMA 2001;286(15):1841-1848.
- Ward C, Hoffman M. Mechanisms of injury and associated forces in high speed rear end impacts. High-Speed Rear Impact TOPTEC, Tempe, Az., Oct 27-28, 1997.
- Griffiths HJ, Olson PN, Everson LI, Winemiller M. Hyperextension strain or "whiplash" injuries to the cervical spine. Skel Radiol 1995;24 (4):263-266.
- Hartling L, Pickett W, Brison RJ. Derivation of a clinical decision rule for whiplash associated disorders among individuals involved in rear-end collisions. Accid Anal Prev 2002;34(4):531-539.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma 1993;34(1):32-39.
- Stabler A, Eck J, Penning R, et al. Cervical spine: postmortem assessment of accident injuries - comparison of radiographic, MR imaging, anatomic, and pathologic findings. Radiology 2001;221(2): 340-346.
Arthur Croft, DC, MS, MPH, FACO, FACFE
Director, Spine Research Institute of San Diego
San Diego, California
Click here for previous articles by Arthur Croft, DC, MS, MPH, FACO.