Many chiropractors specialize in aligning the upper cervical spine; however, medical doctors, dentists and chiropractors alike usually dismiss the adult skull as one fused structure, despite scientific studies to the contrary.1 In fact, the skull is surprisingly pliant and is often affected by tissue strain from the neck.2
The Skull Is Flexible, You Say?
Cranial adjusting has been around since 1929.3 The early investigators, such as Cottam, DC, and Sutherland, DO, looked at skull sutures and reasoned they have movements. Both developed adjustments to affect those movements. But like many ideas before their time, it all got buried in the literature until the late 1970s. That's when John Upledger, DO, and his team at Michigan State did research into the movements of the skull in response to the circulation of the cerebrospinal fluid. They verified that the skull sutures stay moveable throughout life except in certain disease conditions.4
 The range of motion of each joint or suture is small, but when several are involved, the cumulative effect can be quite significant. What can be observed clinically is that the combined rotation of the temporal bones around the occiput can make the mastoid processes misaligned relative to the eyes by up to a half-inch!
The range of motion of each joint or suture is small, but when several are involved, the cumulative effect can be quite significant. What can be observed clinically is that the combined rotation of the temporal bones around the occiput can make the mastoid processes misaligned relative to the eyes by up to a half-inch!
The eyes usually override the vestibular mechanism in cases of minor misalignment. However, when it is severe enough, your patient may complain of dizziness made worse with movements in addition to their suboccipital headache. The body will try to keep the eyes level with the ground and as a result, the upper neck muscles will be hypertonic on one side, and stretched and weak on the other. If the misalignment is severe, the muscles may restrict the vertebral artery unilaterally in what is called the "bow hunter's condition." The patient will complain of dizziness or faintness when turning the head in one direction.5
The dizziness also can be due to the misalignment of the temporal bones taking the two halves of the vestibular system out of alignment with each other.6 This produces a more general sense of imbalance with movement of the head that calms after the patient is still for a few seconds.
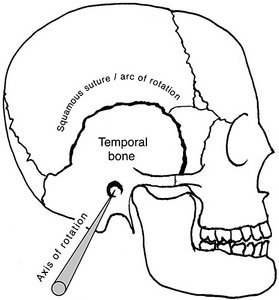 FIG 1 Normal temporal bone movement
The most common pattern of skull misalignment is temporal torsion in which the temporal bones rotate in opposite directions along their axes, the auditory canal. The squamous suture of the skull between the temporal bone and the parietal bone is tapered in such a way as to allow minimal resistance to temporal bone rotation as it slides over the parietal bone. (See Fig. 1 / Fig. 2.)
FIG 1 Normal temporal bone movement
The most common pattern of skull misalignment is temporal torsion in which the temporal bones rotate in opposite directions along their axes, the auditory canal. The squamous suture of the skull between the temporal bone and the parietal bone is tapered in such a way as to allow minimal resistance to temporal bone rotation as it slides over the parietal bone. (See Fig. 1 / Fig. 2.)
A Simple Visual Test
The amount of torsion between the two temporal bones is easily discovered by visual examination of the patient. The doctor faces the patient and places extended index fingers at the base of both mastoid processes where they form an angle with the occiput. Then, by observing the relative level of the fingers to that of the patient's eyes, the approximate amount of functional distortion can be determined. I have seen patients whose mastoid processes are uneven by a half-inch or more (a finger's width) compared to the level of the eyes. (See Fig. 3.)
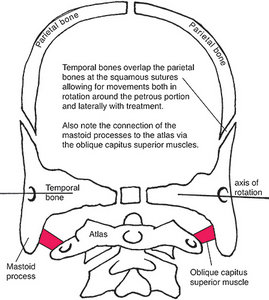 FIG 2 Temporal bone relation to atlas
A simple way to think of cranial torsion is to compare it with what happens in the pelvis. In the pelvis, the two innominate bones rotate around a triangular-shaped bone, the sacrum. Their movements pull on the lower lumbar spine through the connecting iliolumbar and lumbosacral ligaments, causing L5 and L4 to rotate. Similarly, in the skull the two temporal bones rotate around a triangular-shaped bone, the occiput. They pull the atlas and axis through their connections via the suboccipital muscles. This is an extension of the Lovett-Brother relationship.
FIG 2 Temporal bone relation to atlas
A simple way to think of cranial torsion is to compare it with what happens in the pelvis. In the pelvis, the two innominate bones rotate around a triangular-shaped bone, the sacrum. Their movements pull on the lower lumbar spine through the connecting iliolumbar and lumbosacral ligaments, causing L5 and L4 to rotate. Similarly, in the skull the two temporal bones rotate around a triangular-shaped bone, the occiput. They pull the atlas and axis through their connections via the suboccipital muscles. This is an extension of the Lovett-Brother relationship.
Treatment Is Easy
The goal of my approach is to first reduce (as much as possible) the amount of muscle tone in the upper cervical region due to postural compensation. Misalignments of the pelvis often result in torsions of the skull as a compensatory balancing mechanism. So, treatment of skull should begin with realigning the pelvis. Often after realigning the pelvis the skull will straighten on its own.
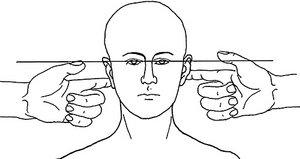 FIG 3 Temporal torsion evaluation test
Use the same test procedure as before. Also look for other spinal misalignments, especially in the T1-2 area (longissimus capitus muscle) and the cervical spine at C4 and below. If all these are functioning well, then the skull can be realigned with a simple procedure dubbed the "ear pull."7
FIG 3 Temporal torsion evaluation test
Use the same test procedure as before. Also look for other spinal misalignments, especially in the T1-2 area (longissimus capitus muscle) and the cervical spine at C4 and below. If all these are functioning well, then the skull can be realigned with a simple procedure dubbed the "ear pull."7
Using the ears as handles, make a light contact with thumb and forefinger close to where the pinna (auricle) meets the skull. (See Fig. 4.) Then gently traction the temporal bones via the ears laterally along the line of the shoulders. The traction should be just barely felt by the patient. Pulling too hard elicits other tissues to protectively guard and contract, preventing the desired treatment.
 FIG 4 Temporal traction "ear pull" technique
Usually it takes about 30 to 40 seconds for the skull sutures to stretch, so be patient. The sensitive practitioner will detect a relaxation of the tissues as a kind of softening or stretching. You also may be aware of the rotation of the bones as they move. As always, you can reassess using the test described above.
FIG 4 Temporal traction "ear pull" technique
Usually it takes about 30 to 40 seconds for the skull sutures to stretch, so be patient. The sensitive practitioner will detect a relaxation of the tissues as a kind of softening or stretching. You also may be aware of the rotation of the bones as they move. As always, you can reassess using the test described above.
Once the skull is realigned, you will find the upper cervical spine may have realigned with it. If not, it will be much easier to adjust, so be gentle. Your patients will think you are a magician when their dizziness and suboccipital headache subsides while they are in your office.
References
- Upledger J, Vredevoogd J. Craniosacral Therapy. Seattle: Eastland Press, 1983.
- Armstrong B, McNair P, Taylor D. Head and neck position sense. Sports Med, 2008;38(2):101-17.
- Cottam C. Use your head: the beginnings of cranial/facial adjusting - the original craniopathy. Digest Chiro Economics, 1988 July/Aug:30-34.
- Upledger J, et al. Op Cit, appendix A.
- Li Y, Peng B. Pathogenesis, diagnosis, and treatment of cervical vertigo. Pain Physician, 2015 Jul-Aug;18(4):E583-95.
- Christine DC. Temporal bone misalignment and motion asymmetry as a cause of vertigo: the craniosacral model. Alt Therapy Health Med, 2009 Nov-Dec; 15(6):38-42.
- Upledger J, et al. Op Cit, pp. 127-128.
Dr. Russ Kalen received his DC degree from Western States Chiropractic College in 1985 and his certification in Craniosacral Therapy with the Upledger Institute in 2005. He practiced in northern California for nearly three decades before retiring in 2014.




