Lumbar disc herniation is a common cause of low back pain, but there are contradictory reports regarding the clinical significance of MRI findings in patients with LBP. The MRI is a very sensitive test for identifying disc lesions, but it is not specific.
MRI vs. Clinical Findings
An interesting observation is that nerve root compression on an MRI does not necessarily produce neurological symptoms or deficits in all patients, but when deficits are present, they correlate well with the presence of root compression on the MRI. That is to say, if a patient has radicular symptoms and neurological deficits, one can expect the MRI to correlate with the clinical findings – but not necessarily the other way around.
According to Janardhana, et al.,1 the presence of neural foramen compromise is more important in determining the clinical signs and symptoms, while the type of disc herniation (bulge, protrusion or extrusion) correlates poorly with clinical signs and symptoms. It seems that the size and extent of the displacement of the disc is not as important as the location and whether or not it compromises the nerve root.
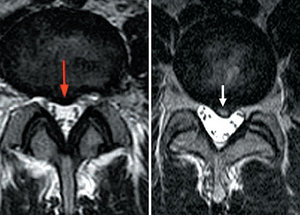 Which patient has lower back pain? The MRI image is sensitive, but may not correlate with clinical symptoms. (See correct answer at end of article.)
Lumbar disc herniation or prolapse is one of the most common causes of low back pain. MRI has provided clinicians a means of viewing the lumbar anatomy in great detail. The pathoanatomical changes in the lumbar disc can be visualized, but there seems to be an issue of which MRI findings are clinical relevant and have diagnostic as well as prognostic value. Borenstein, et al.,2 report that MRI findings are not predictive of the development or duration of low back pain, and that clinical correlation is essential.
Which patient has lower back pain? The MRI image is sensitive, but may not correlate with clinical symptoms. (See correct answer at end of article.)
Lumbar disc herniation or prolapse is one of the most common causes of low back pain. MRI has provided clinicians a means of viewing the lumbar anatomy in great detail. The pathoanatomical changes in the lumbar disc can be visualized, but there seems to be an issue of which MRI findings are clinical relevant and have diagnostic as well as prognostic value. Borenstein, et al.,2 report that MRI findings are not predictive of the development or duration of low back pain, and that clinical correlation is essential.
The question is, which MRI findings are likely to produce symptoms? Studies show that MRI findings with neural foramen compromise and nerve root compression are likely to be more symptomatic than those without neural foramen compromise. The position of the disc herniation can affect the foramen compromise, since central protrusion and extrusions are less likely to cause neural foramen compromise, while centrolateral or far lateral lesions produce neural foramen compromise.
This information is significant when a surgical approach is being considered. For example, consider a patient with a double-level disc herniation: one a disc bulge with neural foramen compromise and the other a central protrusion. The disc bulge with foramen compromise is more likely to cause symptoms.
Facet joint hypertrophy and ligamentum flavum hypertrophy with stenosis of the canal are more commonly seen in patients with neurological deficits, and show a positive association with the MRI findings and neurological deficit. But disc extrusion may or may not be strongly associated with symptoms, depending on the position of the disc extrusion. Whenever there are multiple-level disc lesions, the level associated with neural foramen compromise is most likely to be associated with clinical symptoms and objective neurological deficits.
Takeaway Points
- Not all MRI abnormalities need to have a clinical significance regarding disc displacement.
- The type or size of disc herniation may correlate poorly with clinical signs and symptoms.
- The presence of neural foramen compromise is more important in determining the clinical signs and symptoms.
The issue is that there is a strong tendency to treat disc lesions that are demonstrated on MRI, but these findings may not be the cause of the patient's symptoms, particularly in the case of central disc lesions. I think chiropractors understand the biomechanics of this lesion better than most clinicians, but once the MRI has been performed and a finding demonstrated, there is this tendency to want to "fix it." Conservative management would result in better outcomes, but patients are often not patient.
Aggressive treatment of disc herniation has not improved outcomes. Recent studies document – over approximately a decade – enormous increases in back pain treatment, but these increases have not been accompanied by improvements in patient outcomes or disability rates.
The increase in treatment has been accompanied by a huge increase in the use of MRI for evaluating low back pain. Yet investigators have reported that less than 50 percent of lumbar spinal MRI are considered appropriate. It should be noted that overuse of tests such as MRI is associated with adverse outcomes, such as unnecessary surgeries and increased costs.3
References
- Janardhana AP, Rajagopal, Rao S, Kamath A. Correlation between clinical features and magnetic resonance imaging findings in lumbar dis prolapse. Indian J Orthop, 2010 Jul-Sep;44(3):263-269.
- Borenstein DG, O'Mara Jr. JW, Boden SD, Lauerman WC, et al. The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: a seven-year follow-up study. J Bone Joint Surg (U.S.), 2001;83:1306-11.
- Emery DJ, et al. MRI overused for low back pain. JAMA Internal Medicine, March 25, 2013 (epub ahead of print).
Answer: image on the left (red arrow).
Click here for more information about Deborah Pate, DC, DACBR.





