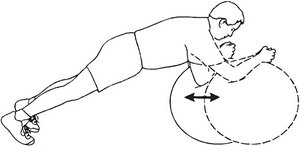
 Figure 1
In day-to-day practice, the thoracolumbar (T/L) fascia is considered an important part of the exam in relation to a possible source of low back and shoulder pain.
Figure 1
In day-to-day practice, the thoracolumbar (T/L) fascia is considered an important part of the exam in relation to a possible source of low back and shoulder pain.
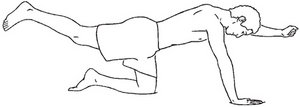 Figure 2
The thoracolumbar fascia also responds to heat treatments. Therefore, deep tissue laser, especially those with a "track ball" applicator, allow you to provide myofascial release massage to loosen up adhesions within the muscle. In addition to the above modalities, there is a new treatment available utilizing "fascial traction." This treatment is based on negative pressure which provides pulling the soft tissue which makes it different than the above modalities. Rather than pushing into the skin, this modality uses a hand held device placed on the skin that uses suction to pull the fascia and soft tissues. The device can be used with passive and or active movements. Fascial traction can be performed to the fascia and lymphatic system with varying amounts of suction along with a glide, stroke, torque, pull, vibration, all in a multi-planar nature. The practitioner can control the intensity of the desired suction (negative pressure) from 80 mmHg to 250 mmHg.
Figure 2
The thoracolumbar fascia also responds to heat treatments. Therefore, deep tissue laser, especially those with a "track ball" applicator, allow you to provide myofascial release massage to loosen up adhesions within the muscle. In addition to the above modalities, there is a new treatment available utilizing "fascial traction." This treatment is based on negative pressure which provides pulling the soft tissue which makes it different than the above modalities. Rather than pushing into the skin, this modality uses a hand held device placed on the skin that uses suction to pull the fascia and soft tissues. The device can be used with passive and or active movements. Fascial traction can be performed to the fascia and lymphatic system with varying amounts of suction along with a glide, stroke, torque, pull, vibration, all in a multi-planar nature. The practitioner can control the intensity of the desired suction (negative pressure) from 80 mmHg to 250 mmHg.
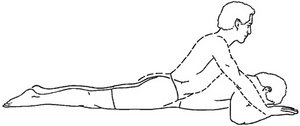
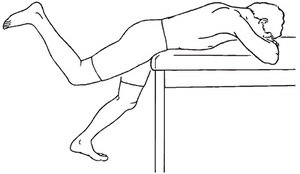 Figure 3
The usual fascial treatment approach is to slowly sink into the layer of the body until you meet a resistance barrier. This technique is the opposite because it tests for restrictions by pulling the skin and fascia away (through suction). The device allows us to test while seeing and feeling the glide (or lack of glide) of the fascia. The lighter setting (80 to 150 mmHg) of the suction is used in the early stages of inflammation, lymphatic drainage and for the superficial fascia. Higher settings (150 to 250 mmHg) of suction will influence the deep fascial compartments and vessels. I especially like that the hand held device allows me to visually evaluate the symmetrical or asymmetrical movement of fascial tension. Treatment of restricted fascia is applied using the suction device coupled with oblique turns and twists, transverse, circular and kneading motions.
Figure 3
The usual fascial treatment approach is to slowly sink into the layer of the body until you meet a resistance barrier. This technique is the opposite because it tests for restrictions by pulling the skin and fascia away (through suction). The device allows us to test while seeing and feeling the glide (or lack of glide) of the fascia. The lighter setting (80 to 150 mmHg) of the suction is used in the early stages of inflammation, lymphatic drainage and for the superficial fascia. Higher settings (150 to 250 mmHg) of suction will influence the deep fascial compartments and vessels. I especially like that the hand held device allows me to visually evaluate the symmetrical or asymmetrical movement of fascial tension. Treatment of restricted fascia is applied using the suction device coupled with oblique turns and twists, transverse, circular and kneading motions.
If you are familiar with treating scar tissue, adhesions, fascial restrictions, etc, you know that even light stroking, instrument assisted tools, vibration and percussion and many other therapies have definite therapeutic effects. It makes sense that allowing oxygen and blood flow to be brought to dense facial areas will enhance therapy.
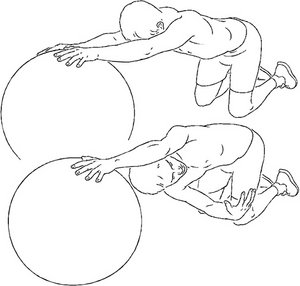 Figure 4
Applying the Rehab Model
Figure 4
Applying the Rehab Model
I find that I can couple hands-on therapy with the deep muscle stimulator, radial pulse wave therapy and/or laser, along with teaching patients how to lengthen the overactive muscles and strengthen the underactive muscles. If the patient is guided to actively move an area related to the thoracolumbar fascia while applying therapy, each time muscle contraction takes place blood is forced through the veins, and the absorption of lymph is increased through the lymphatic vessels, accelerating the flow of the arterial blood with its fresh supply of nutriment and oxygen. Some of the positions I put patients in while treating thoracoclumbar fascial dysfunction are remedial repetitive movement exercises. For the acute and subacute patients, I can experiment with prone press-ups (Fig. 1), birddog (Fig. 2), and on the forearm and knees hip extension patterns (Fig.3).
When a patient comes in with pain related to the thoracolumbar area, in addition to testing range of motion and palpation, I check for pronation issues, test gait and check the Janda hip extension and abduction movement patterns because the body often compensates for weakness of the gluteus maximus with an over-action of the erector spinae to extend the hip.
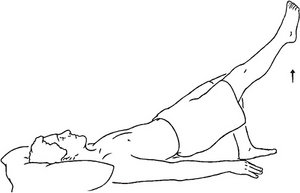 Figure 5
Whether or not the patient has a history of spinal degeneration, facet syndrome or disc irritation, focusing on breaking up T/L fascial restrictions, improving muscle firing-timing training and strength training can create greater muscle control that will then act as a shock absorber to decrease and slow the degenerative process in the low back. Additional T/L treatment poses and remedial take-home rehab exercises to consider:
Figure 5
Whether or not the patient has a history of spinal degeneration, facet syndrome or disc irritation, focusing on breaking up T/L fascial restrictions, improving muscle firing-timing training and strength training can create greater muscle control that will then act as a shock absorber to decrease and slow the degenerative process in the low back. Additional T/L treatment poses and remedial take-home rehab exercises to consider:
- Tight hip flexors need to be released. Think of poses that target the quads, psoas and iliacus. I frequently train patients in half kneeling poses.
- The thoracolumbar erector spinae should be relaxed and stretched using appropriate techniques. I especially like "thread the needle" (Fig. 4). exercises on all fours for restricted lower thoracic regions.
- Partial wall squats leaning against a stability ball to train proper knee tracking improve gait patterns.
- The gluteal muscles and abdominals need to be facilitated and strengthened. You can perform gluteal exercises by placing the pelvis in neutral and perform supine bridges. Start with two-legged bridges with the patient pushing into there heels while lifting the pelvis. You can progress to one-legged bridges (Fig. 5).
- For abdominals strength and stability, static planks and/or ab roll-outs are good starters (Fig.6).
Releasing fascial restrictions in the office is only half the battle. I make sure I communicate to patients that exercise makes all the difference in outcome. When testing for fascial dysfunction, first test for range of motion restrictions and palpate for dense tissues. Correct the dense tissues using hands-on therapy, deep tissue warm laser, deep muscle stimulator and/or radial shock wave therapy. During the in-office session, teach the patient what to do for there at-home exercise, then re-test there ROM and palpation findings. When using this process, within session reassessment has been shown to predict between–session improvement. If immediate post-treatment audit of mechanical sensitivities showed improvement, patients were at least 3.5 times more likely to have between-session improvement as well. (Hahne, A et al. 2004; Do within-session changes in pain intensity and range of motion predict between-session changes in patients with low back pain? Australian Journal of Physiotherapy, 50, 17-23). Exercise Photo Reference: Visual Health Information www.vhikits.com/products/software/pckitsdesktop.aspx.
Click here for more information about Jeffrey Tucker, DC, DACRB.