Before I discuss the basic principles of roentgenographic technique, I would like to remind the reader that the basic technique for performing a chest study is not the same as performing a thoracic spine series. If a small lesion is present in the lung fields on the thoracic spine study, we are obligated to follow up with at least a chest study to evaluate that lesion. If one is only concerned with the thoracic spine region, just collimate enough to view the thoracic spine-don't include the lung fields!
The basic principles of roentgenographic technique for performing a chest film are as follows:
- Position the patient so that the central ray is at approximately T-6 and that there is no rotation. The scapulae should be rotated anteriorly as to be projected free of the lung field. It is assumed that the PA chest is taken with the patient's back to the tube or in the PA position, unless otherwise labeled on the film; also, it is assumed that the film focal distance is 72 inches.
- Respiration must be fully suspended, preferably at close to total lung capacity (full inspiration).
- Exposure factors should be such that the resultant film permits faint visualization of the thoracic spine and disc spaces, so that lung markings behind the heart are clearly visible; exposure should be as short as possible. (Remember, the patient is holding his or her breath.)
- To achieve consistently high-quality chest films, a high kilovoltage technique (110-150 kVp) and short exposure time, a tenth of a second or less, and a slower-speed cassette are generally recommended.
- The lateral view is performed using the same focal distance (72 inches) and high kilovoltage. The patient should be standing with the left side closest to the cassette, with the arms positioned out of the way of the chest. The central rag is in the axillary region, in full inspiration.
If you are going to perform chest studies, it is a good idea to have one detail cassette, and to reserve that for chest studies only. Rare earth screens are not particularly good for chest films because they were not developed for exposures of high kVp techniques. The crystals are too large, and the fine detail needed for evaluating the lung field is lost.
There are many roentgenographic technique references available that will cover techniques for chest studies, but most of the time, a simple PA and lateral should be sufficient to evaluate the lungs and mediastium. If there is a lesion on the chest film, most of the time a CT will be performed to localize the lesion unless previous films are available for comparison. Most facilities perform chest studies with digital radiography, so it is easy to maintain image quality and review previously performed studies.
I personally do not perform chest studies in the office any more, as the digitized imaging available presently is far more consistent, and many times superior to what I can perform in the office.
|
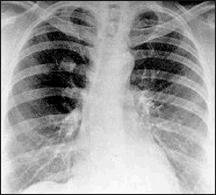
| Fig. 1: Posteroanterior chest roentgenogram showing a 2 cm solitary pulmonary nodule in the right upper lobe. |
Enough of the technique. Let's review the radiographic parameters of a solitary pulmonary nodule (SPN). First, it must be a radiographic opacity. The lesion must be singular, surrounded by normal lung, and not be involved with obstructive atelectasis or hilar enlargement (Figure 1). In general, the lesion should be nodular. Various studies through the last few decades have included lesions of 1-6 cm as SPNs; however, more recent series have restricted the discussion to lesions 1-4 cm in diameter. The importance of narrowing the diagnostic discussion to lesions of this size is to exclude large lesions that are uniformly malignant. Most stage I lung cancers are within the definition of SPN. The five-year survival rate for resection of stage I bronchogenic carcinoma is 75 percent and over 80 percent for lesions <3 cm.
There are a multitude of benign and malignant processes that may present as an SPN on a chest radiograph. Table 1 lists the more common diagnoses, though there are many processes that uncommonly present in this manner.
Before the advent of CT, 60 percent of these small lesions surgically resected were benign. More recently, studies utilizing CT have reduced the number of benign nodules resected to 20-40 percent. The most common benign causes of SPNs are granulomas from histoplasmosis, coccidioidomycosis, and mycobacteria. Hamartomas are the most common benign neoplasms and constitute approximately 10 percent of benign nodules resected.
Bronchogenic carcinoma is, by far, the most common malignant lesion in surgical series of SPNs. Adenocarcinoma and large cell carcinoma account for more peripheral nodules than squamous and small cell carcinomas, although all histologic types of lung cancer may present as an SPN. Metastatic lesions from nonlung primary tumors constitute about 10-30 percent of resected malignant nodules. The most frequent sources of metastasis are squamous carcinomas of the head and neck, and adenocarcinomas of the breast, kidney and colon.
Patients with SPN rarely have symptoms attributable to the nodule, and so the detection of the SPN is usually serendipitous. The plain chest roentgenogram usually defines the presence and appearance of the SPN unless discovered on CT or other radiographic imaging performed for another purpose. The importance of reviewing previous chest radiographs cannot be overemphasized. Every effort to obtain previous chest films should be made, as a lesion remaining unchanged over a two-year period is highly likely to be benign. The previous chest film may establish growth of the nodule and indicate a high likelihood of malignancy, prompting resection.
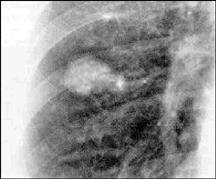
The presence of calcification within a nodule on plain film, tomography, or a CT is a reliable indicator that the nodule is benign. Classically, granulomas may show a laminated or a concentrically ringed calcification pattern. Other benign calcification patterns include central, diffuse, and "popcorn ball," which may be seen with hamartomas (Fig 2). About 10 percent of malignant lesions show evidence of calcification on plain chest film, and eccentric calcification should raise suspicion of malignancy.
|
| Fig. 2: Posteroanterior chest roentgenogram showing a 2 x 2.5 cm nodule with "popcorn ball" calcification, which is indicative of hamartoma. |
Great strides have been made in the identification of nodules as benign utilizing CT. Chest CT is more sensitive than plain film or tomography in the detection of calcium, and multiple nodules may be identified. The standard CT is more sensitive in identifying calcium as well as detecting hamartomas by the presence of fat.
There are a number of imaging techniques that offer exciting advances in evaluation of SPNs. Positron emission tomography (PET) scanning with F-18 fluorodeoxyglucose has been shown to be accurate in differentiating benign focal pulmonary abnormalities from malignant ones. Despite the technique's accuracy, PET scanning is expensive and not widely available. Magnetic resonance imaging with Gd-DTPA may also be helpful in differentiating between malignant and benign lesions.
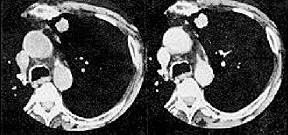
The most potentially widely available and sensitive new imaging modality for the evaluation of SPNs is CT contrast enhancement (Fig 3). The test involves a thin-section density assessment of uncalcified lung nodules before and after the administration of a conventional iodinated contrast material. Malignant neoplasms enhanced significantly more than granulomas and benign neoplasms. The benign lesions that showed significant enhancement were hamartomas and active granulomas. The degree of enhancement was related to the amount of central vascular staining in histologic evaluation of surgical specimens. The overall accuracy of 93 percent establishes CT contrast enhancement as an invaluable tool in the evaluation of indeterminate SPNs.
|
| Fig. 3: Thin-section CT scan before (left) and after (right) intravenous contrast injection. The nodule is enhanced 49 Hounsfield units. Resection showed squamous carcinoma. |
Ideally, all malignant SPNs would be resected shortly after detection, and all benign lesions would be identified without surgical intervention. Recent radiographic advances move physicians further toward this degree of precision. The radiographic discovery of an SPN immediately raises concern that malignancy may be present. Careful assessment should include a thorough history and physical examination with attention to age, smoking history, prior history of malignancy, and other systemic clues to the identity of the nodule (e.g., Wegener's granulomatosis or rheumatoid arthritis). Review of former films may establish the nodule as benign by stability over time or highly likely malignant by evidence of growth. Fluoroscopy and tomography may be helpful in clarifying that a suspected nodule is nonexistent or by identifying calcification. If the nodule is indeterminate and less than 3 cm in diameter, thin-section CT, dual kV CT, or phantom densitometry may help visualize calcium or infer benignancy by density. Contrast CT is highly accurate in identifying benign and malignant lesions by presence or absence of density enhancement. Where available, PET scanning may also be used. For nodules greater than 3 cm that are known or presumed to be malignant, surgical resection follows staging CT of the chest and upper abdomen.
Nodules less than 3 cm that remain indeterminate after radiographic studies call for a decision between observation, biopsy, and thoracotomy. Observation involves careful follow-up with serial chest radiographs every three months for the first year, and every six months for the second year, and yearly thereafter if benignancy is not clearly established, to exclude the possibility of a slow-growing malignancy. The occasional nodule that is not clearly demonstrated on plain chest film may require serial observation with CT. Bronchoscopy may be helpful in obtaining tissue in certain clinical settings; however, it is limited by its relative inability to make specific benign diagnoses. Biopsy may help avoid resection only when a benign diagnosis is obtained. Biopsy may also be helpful in establishing a malignant diagnosis in the high-risk medical patient in whom surgery would be indicated only for known malignancy.
A high probability of malignancy is expected in large nodules and among older smokers. Resection would seem indicated under these circumstances. However, in young, nonsmoking patients, nodules are likely benign, and observation would seem to offer the best risk: benefit assessment. Often the best management of an indeterminate SPN may be unclear, and this emphasizes the need to educate the patient and involve the patient in the decision making process. Further advances in imaging techniques show promise in easing the decision making and reducing the "incision making."
References:
- Lesson 18, Volume 11-Solitary Pulmonary Nodule By David E. Midthun,MD http://www.chestnet.org/education/pccu/best/lesson18-11.html.
- Great site to learn more: http://www.chestnet.org/education/pccu/best/bestintro.html
Deborah Pate,DC,DACBR
San Diego, California
Click here for more information about Deborah Pate, DC, DACBR.