When evaluating a shoulder and realizing that there might be a torn labrum, the conservative practitioner often becomes thwarted since, except for surgery, there is no way to repair a torn labrum.
A recent paper concluded, "A trial of non-operative treatment may be considered in patients with the diagnosis of isolated superior labral tear."2 Although 71 percent of patients returned to the same or better levels of participation, only 10 of the 15 overhead athletes (67 percent) returned to their overhead sport at the same or higher level. Each had an initial three-month course of non-operative treatment before operative treatment was considered. Rehabilitation consisted of nonsteroidal anti-inflammatory drugs and a posterior capsular stretching and strengthening program.
Another paper explained the possible reasoning behind the success of posterior inferior capsular stretching and scapular open- and closed-chain exercises.3 The type II SLAP lesion, whereby the superior labrum and biceps anchor are detached from the glenoid rim, is the most common type of labral lesion in overhead athletes as well as non-athletes.
Tennis and baseball players often develop an increase in external rotation with an equal decrease in internal rotation. If there is a greater loss of internal rotation compared to external rotation, referred to as glenohumeral internal rotation deficit (GIRD), labral tears may result.4 In GIRD, there is usually a tight, contracted posterior capsule from thickening of the capsule that develops due to tensile overload occurring during the deceleration phase. During the cocking phase, the humeral head moves to a more posterior superior position, which can lead to internal impingement of the labrum between the posterior superior glenoid and the humerus, resulting in degenerative labral changes. This posterior shifting of humeral head might be more of a cause of anterior shoulder instability than stretching of the anterior capsule.
 Figure 1: The posterior inferior capsule stretch.
A tight posterior capsule can lead to both anterosuperior and posterosuperior migration of the humeral head. As external rotation increases, shear forces at the biceps anchor and posterior superior labral attachment are increased, causing the biceps to assume a more vertical and posterior position, resulting in a torsional force and causing a "peel back" of the labrum. This results in a type II labral tear.3
Figure 1: The posterior inferior capsule stretch.
A tight posterior capsule can lead to both anterosuperior and posterosuperior migration of the humeral head. As external rotation increases, shear forces at the biceps anchor and posterior superior labral attachment are increased, causing the biceps to assume a more vertical and posterior position, resulting in a torsional force and causing a "peel back" of the labrum. This results in a type II labral tear.3
Patients with suspected SLAP lesions who have GIRD must be treated with stretching of their posterior inferior capsule. Figure 1 depicts stretching of the posterior inferior capsule by having the patient horizontally adduct the arm and, at the same time, elevate the shoulder. Figure 2 is the "sleeper stretch," accomplished by the patient lying on their side with the elbow and shoulder at 90° flexion and passively internally rotating the shoulder.
 Figure 2: The "sleeper stretch."
Scapular dyskinesis is another factor related to labral function. When evaluating the standing patient, the shoulder will be low (usually on the dominant side) compared to the opposite side. Notice if the dominant-side scapula shows a prominence of the inferior medial border, with the superior border and acromion appearing less distinct. There may be a tight pectoralis minor, short head of the biceps and shortening of the pectoral fascia tilting the coracoid inferiorly. This is responsible for anterior shoulder pain and upper trapezius pain, and is related to a protracted scapula. Have the patient flex the shoulders forward up and down three to five times with a three- to five-pound weight in their hands. See if the medial border of the scapula becomes more prominent.
Figure 2: The "sleeper stretch."
Scapular dyskinesis is another factor related to labral function. When evaluating the standing patient, the shoulder will be low (usually on the dominant side) compared to the opposite side. Notice if the dominant-side scapula shows a prominence of the inferior medial border, with the superior border and acromion appearing less distinct. There may be a tight pectoralis minor, short head of the biceps and shortening of the pectoral fascia tilting the coracoid inferiorly. This is responsible for anterior shoulder pain and upper trapezius pain, and is related to a protracted scapula. Have the patient flex the shoulders forward up and down three to five times with a three- to five-pound weight in their hands. See if the medial border of the scapula becomes more prominent.
If there is scapular protraction and loss of the normal posterior tilting of the scapular (therefore increased glenoid ante-tilting) as the humerus moves into external rotation, the scapula may be moving into internal rotation. The scapula may be seen protracted at rest, suggesting that there will be increased internal impingement (humeral head shifting against posterior superior glenoid) and shear during external rotation. Excess scapular protraction may create compensatory increased glenohumeral external-rotation angulation, resulting in excessive posterior compression. This may increase "the risk of injury, not only to the posterior superior labrum, but also to the undersurface of the posterior supraspinatus tendon and anterior inferior capsular structures."3
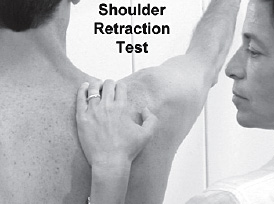 Figure 3: The scapular retraction test for assessing the negative effects of scapular protraction.
Check the negative effects of scapular protraction by performing the scapular retraction test (Figure 3). Stand behind the patient and press down on the medial border of the scapula to prevent anterior tilting. At the same time, test the previously tested supraspinatus muscle, which may now demonstrate increased strength with scapular stabilization. By positioning the glenoid in a less ante-tilted position, internal impingement and posterior shear may be decreased.
Figure 3: The scapular retraction test for assessing the negative effects of scapular protraction.
Check the negative effects of scapular protraction by performing the scapular retraction test (Figure 3). Stand behind the patient and press down on the medial border of the scapula to prevent anterior tilting. At the same time, test the previously tested supraspinatus muscle, which may now demonstrate increased strength with scapular stabilization. By positioning the glenoid in a less ante-tilted position, internal impingement and posterior shear may be decreased.
Besides stretching the posterior capsule, work on strengthening the rotator cuff and scapular stabilizers. For the scapula, closed-chain exercises should be done for all motions, followed eventually by open-chain exercises. Stretching and fascial manipulation of the anterior shoulder muscles and fascia should be performed if indicated.
References
- Hammer W. "Latest Test for Detecting SLAP Lesions." Dynamic Chiropractic, Jan. 1, 2008;26(1).
- Edwards SL, Lee JA, Bell J-E, et al. Nonoperative treatment of superior labrum anterior posterior tears: improvements in pain, function, and quality of life. Am J Sports Med, 2010;38(7):1456-61.
- Adams GD, Safran MR. Diagnosis and management of superior labrum anterior posterior lesions in overhead athletes. Br J Sports Med, 2010;44:311-8.
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy, 2003;19:404-20.
Click here for previous articles by Warren Hammer, MS, DC, DABCO.





