I have noticed (and I suspect you have, too) that the thoracolumbar (T-L) junction is almost always tight in lower back pain patients. I used to think this was a compensation, something to be noted and maybe treated, but not a key restriction; not a source of lumbar and pelvic pain.
Let's learn more about the condition, including how to assess and treat it. This is another in my "most missed" series. When I say "most missed," I am usually talking about patterns I have noticed that are not commonly recognized. This is one I missed for 31 years.
Robert Maigne is a French MD who practices musculoskeletal medicine, including manipulation and injection procedures. His papers are available for review on the Web site of the French Society of Orthopaedic and Osteopathic Manual Medicine. (Yes, there is an English version.)1 Look at the series of papers on the thoracolumbar junction.
There is also an interview with Robert Maigne online on another site;2 he discusses this condition and shares his own story as a pioneer in manipulative medicine. I found this interview fascinating, particularly in terms of Maigne's thinking process. He notes that most upper thoracic pain comes from the lower cervical spine. When asked if the lower thoracic syndrome is a facet syndrome, he gives a well-thought-out answer; basically, he says there are multiple sources of pain around a joint, not just the facets. We don't really know the exact source, but we do know how to assess and treat.
In the same interview, he describes Maigne's syndrome as usually unilateral lower back pain frequently mistaken for back pain of lumbosacral origin. There may also be abdominal, testicular or gynecological pain syndromes related to the T-L junction or to irritation of the nerves from L2-3; the lateral femoral cutaneous nerves. Maigne states that the patient never complains of pain at the T-L junction. Radiographs are usually non-contributory.
The Relevant Anatomy
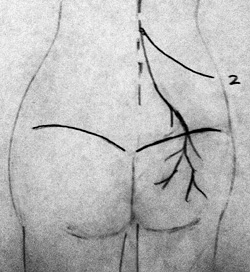 The superior cluneal nerves leave the spine at the T-L junction and provide sensory supply to the lower lumbar and gluteal area. Note #2, the lateral femoral cutnaneous nerves, wrapping around (should actually be exiting slightly lower in the spine).
Maigne points out that sensory innervation of the flank, of the tissues over the lower lumbar spine and the pelvis, comes from the superior cluneal nerves, which originate between T10 and L2. (Maigne notes in the interview referenced above that the anatomy books state that the nerve supply to gluteal area is from L2-3 only, so he did his own dissections to establish the broader origin of the superior gluteal nerves.) These sensory nerves come out of the T-L junction and go down across the lower back, crossing over the pelvic brim into the buttock.
The superior cluneal nerves leave the spine at the T-L junction and provide sensory supply to the lower lumbar and gluteal area. Note #2, the lateral femoral cutnaneous nerves, wrapping around (should actually be exiting slightly lower in the spine).
Maigne points out that sensory innervation of the flank, of the tissues over the lower lumbar spine and the pelvis, comes from the superior cluneal nerves, which originate between T10 and L2. (Maigne notes in the interview referenced above that the anatomy books state that the nerve supply to gluteal area is from L2-3 only, so he did his own dissections to establish the broader origin of the superior gluteal nerves.) These sensory nerves come out of the T-L junction and go down across the lower back, crossing over the pelvic brim into the buttock.
One particular gluteal tender point, 7-10 cm lateral to the midline, is right below the iliac crest. Just superior to this gluteal tender point is an osteofibrous tunnel that the nerve comes through. Tunnels tend to be problematic areas; nerves can get impinged. This phenomenon, this particular tender point, is probably a double-crush syndrome. The impingement appears to occur at the spinal origin of the cluneal nerves, from T10 through L2, with peripheral nerve impingement occurring most likely at the tunnel.
I have been trying to normalize that particular gluteal tender point with multiple approaches for years and years. I have thought of it as an iliosacral separation. I have done all kinds of manual approaches to that spot as a muscular knot, including Graston technique, counterstrain and myofascial release. I have attempted to clear the fixation patterns throughout the pelvis and lower lumbar spine. All of these approaches have occasionally worked, but none changed that tender point consistently. Once I read Maigne's paper and started using the approach outlined below, the tender point more consistently disappeared and stayed gone.
An Assess, Treat and Reassess Protocol for This Syndrome
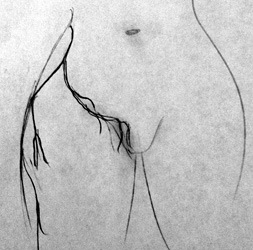 The course of the lateral femoral cutaneous nerves, providing sensory supply to the gluteus medius area and the groin.
If I have anything unique to offer on this topic, here it is. This is a simple assess, treat, reassess protocol. I love that we often can get immediate feedback about whether we are making a difference. I also love conditions that respond in a clear-cut way to manipulation. First, find that trigger point, the knot, and associated ones along the inferior margin of the iliac crest. Mark them. If you don't mark this spot, you may not be able to go back to the exact spot. Next, go up to the T-L junction, assessing the paraspinal area between T10 and L2. Palpate it, move it. Does it show abnormal sensitivity and tenderness, and a lack of motion? Yes, the whole area tends to be tight; ignore that for the moment and look for the signal within the noise.
The course of the lateral femoral cutaneous nerves, providing sensory supply to the gluteus medius area and the groin.
If I have anything unique to offer on this topic, here it is. This is a simple assess, treat, reassess protocol. I love that we often can get immediate feedback about whether we are making a difference. I also love conditions that respond in a clear-cut way to manipulation. First, find that trigger point, the knot, and associated ones along the inferior margin of the iliac crest. Mark them. If you don't mark this spot, you may not be able to go back to the exact spot. Next, go up to the T-L junction, assessing the paraspinal area between T10 and L2. Palpate it, move it. Does it show abnormal sensitivity and tenderness, and a lack of motion? Yes, the whole area tends to be tight; ignore that for the moment and look for the signal within the noise.
Find the direction of maximum tenderness and the direction of maximal fixation. Correct the restricted and tender T-L junction segments with your own combination of manipulation, mobilization and soft-tissue therapies. The most common pattern appears to be a lack of extension and lack of lateral bending toward the involved side. It can be a lack of extension and lateral bending away. Sometimes, the pattern is more like a counter-rotation pattern with restriction of two segments on either side of the spine, one above the other.
After spinal correction, immediately go back to the gluteal tender point. It usually will have become much softer, much less tender. I was amazed when I started doing this; it really works well and fairly consistently. If the trigger point is significantly less tender, you know that the T-L junction is an important and contributory source of the pelvic and lumbar issues.
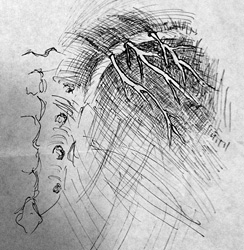 (After Maigne; sacrum on left, right iliac crest to the right). Note the osteofibrous tunnels the superior cluneal nerves come through and their supply to the skin, just below the iliac crest.
Here is a recent case history to illustrate. I told you I am embarrassed that I wasn't seeing this pattern. The patient was an active 60-year-old female who, while ice skating, banged into the side of the rink, bruising her left flank (clue one: injury to T-L area). She started having pain in the left lower back and left gluteal region.
(After Maigne; sacrum on left, right iliac crest to the right). Note the osteofibrous tunnels the superior cluneal nerves come through and their supply to the skin, just below the iliac crest.
Here is a recent case history to illustrate. I told you I am embarrassed that I wasn't seeing this pattern. The patient was an active 60-year-old female who, while ice skating, banged into the side of the rink, bruising her left flank (clue one: injury to T-L area). She started having pain in the left lower back and left gluteal region.
I tried everything (and she was a motivated exerciser). I released the QL; I did visceral to the kidney. The SI was unstable; I addressed that and she did four sessions of prolotherapy to the lumbosacral and SI area. We did extensive trigger point and dynamic Graston to the gluteals, etc. End result: Eighteen months later, she was still hurting in the same places; the left SI area primarily.
After I read Maigne's paper, the patient happened to come in and did show the classic trigger point, 7 cm lateral to midline in the upper gluteals. She did indeed show restriction at the left T-L junction. I corrected, via mobilization and manipulation, the T-L restrictions. There was immediate reduction in the trigger-point nodularity and tenderness. A week later, she was markedly improved - finally.
Other Contributory Tissues
As usual, when it comes to dysfunction of the human form, there is not one simple solution. Although addressing the T-L junction can be profound, there obviously can be other contributors to lower back pain and to this gluteal tender point. One obvious one is thinking of the gluteal tender point as a tunnel syndrome, the distal half of the double crush. In this case, soft-tissue techniques or dry needling applied to the area of tenderness and associated points nearby may help break up the knot in the tender area.
Lateral femoral cutaneous syndrome is another referred pain pattern related to the upper lumbar spine. The sensory nerves from L2-3, as pictured in this article, wrap around and supply the skin over the lateral gluteus medius, as well as into the groin.
The psoas and diaphragm meet at the thoracolumbar junction. The superior cluneal nerves traverse through the psoas. If the psoas or diaphragm is dysfunctional, it can create problems or reinforce dysfunction at these spinal levels.
The self-correction for this restriction could be attention to breathing and getting better extension into the thoracolumbar junction with a foam roller or similar extension exercise. Any back pain will overactivate the long mobilizer muscles and inhibit the deep stabilizers. Rehab needs to address both the tightness of the erectors and the weakness/inhibition of the core, the deep stabilizer muscles. The quadratus lumborum is another muscle that will need rehab for this condition.
Maigne discounts the possibility that the iliolumbar ligament could be a source of this pain, stating that the ligament originates on the anterior portion of the iliac crest, and that it is difficult or impossible to palpate. The trigger point in question is clearly just below the iliac crest, on the posterior side.
I have a different take on this. I agree that this gluteal trigger point is not directly over the iliolumbar ligament. But I do think that the iliolumbar ligament can be quite clinically significant and can be another contributor to referred pain into the buttock. You can palpate and treat this ligament. If you position the patient correctly by slacking the area and go deeply enough, you can provide cross-friction to both the origin and insertion of the iliolumbar ligament. I have seen cases in which the gluteal tender point did not release after mobilizing the T-L junction, and did release after I cleared tender points in the iliolumbar ligament.
Warren Hammer wrote an article 13 years ago for Dynamic Chiropractic about the phenomena of superior cluneal nerve entrapment.3 As usual, he got there way before me. (Warren focused on the soft-tissue aspect of this condition.) A Web site called Chiropractic-Help.com also discusses this topic. The site features a detailed section on Maigne syndrome.4
I find it hard to believe that after 31 years of treating and assessing lower backs, I just added this significant piece, assessing the thoracolumbar junction, to my search pattern. The critical information to understand is that the gluteal tender point is related to the T-L junction restriction.
Author's note: Special thanks to David Fishkin, DC, of the Dry Needling Institute, for calling my attention to the Maigne papers on this topic.
References
- Web site of the French Society of Orthopaedic and Osteopathic Manual Medicine: www.sofmmoo.com/english_section/accueil_english_section.htm
- Interview with Robert Maigne regarding Maigne's syndrome. www.maitrise-orthop.com/corpusmaitri/interview/maigne/maigneus.shtml
- Hammer W. "Superior Cluneal Nerve Entrapment - An Overlooked Cause of Low Back Pain." Dynamic Chiropractic, May 4, 1998.
- Additional information on Maigne's syndrome. www.chiropractic-help.com/maignes-syndrome.html
Click here for more information about Marc Heller, DC.





