The tibialis posterior is the deepest, strongest and most central muscle of the leg, with fibers originating from the tibia, fibula and interosseous membrane. The tendon of the tibialis posterior forms in the distal third of the leg and angles sharply forward as it passes posterior to the medial malleolus.
To improve its efficiency, tibialis posterior's tendon rotates more than 45 degrees before it attaches,1 allowing the tendon to store and return energy like a spring membrane. When working properly, the tibialis posterior functions to store energy as the arch begins to flatten and returns this energy to elevate the arch during propulsion.
Given the multiple attachment points and powerful tendon, when the tibialis posterior tendon is injured, the biomechanical stability of the entire foot can be severely compromised. The integrity of the tibialis posterior tendon may be affected by diabetes, steroid use, hypertension, autoimmune disorders and previous trauma. Biomechanical factors such as obesity, tarsal coalition and various neuromuscular disorders also may play a role in weakening the tendon.
Symptoms / Progression
Early symptoms associated with tibialis posterior tendinitis include pain around the posterior aspect of the medial malleolus, along with foot and ankle fatigue while walking, especially on uneven surfaces. Over time, a characteristic swelling of the tendon forms between the navicular tuberosity and the medial malleolus, and the patient often develops lateral ankle pain because the progressive rearfoot valgus increases lateral talocalcaneal impingement; i.e., eversion of the calcaneus causes the lateral aspect of the talar dome to compress the corresponding surface of the lateral tibial plafond.
Clinically, continued tibialis posterior tendinopathy produces progressive deformity of the foot in which the forefoot abducts and the midfoot collapses. This is often evidenced by the "too-many-toes" sign, in which a greater number of lateral toes can be seen when viewed from behind. Another clinical sign of tibialis posterior insufficiency is the poorly stabilized first ray collapses when the patient attempts to perform a single-limb heel raise.2
The progressive deformity associated with tibialis posterior tendon dysfunction is divided into four stages. In the first stage, the tendon is inflamed, but not lengthened; and there is no sign of altered foot shape. The individual complains of medial ankle pain with single-leg heel raises, and mild weakness is noted when resisting rearfoot inversion. In the second stage, a flexible flatfoot is developing and there is an increased range of rearfoot eversion and forefoot abduction, resulting in a positive too-many-toes sign. There is marked weakness of tibialis posterior and the patient is unable to perform a single-leg heel raise without significant discomfort.
Conservative Treatment
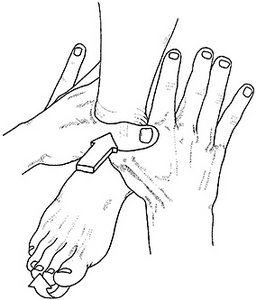 Fig. 1. Manipulation to restore forward glide of the calcaneus beneath the talus. In this adjustment, the plantar heel is stabilized by friction from the examining table while the crossed thumbs apply a posterior shear force through the talus. Initially, a force is applied gently, causing the talus to glide posterior on the fixated calcaneus. When performed properly, a smooth gliding motion should be felt, and the forefoot should lift slightly off the examining table. This manipulation should be performed with as little force as possible to avoid stressing the tibialis posterior tendon.
Nonoperative treatment for first- and second-stage tendon dysfunction consists of either stock or custom-made orthotics manufactured with large varus posts. The orthotic shell is usually made from soft materials, because patients with tibialis posterior tendinitis often find the harder shells uncomfortable (perhaps because the weakened tibialis posterior is unable to prevent the midfoot from jamming into the orthotic shell). A large varus post is essential, as it effectively reduces symptoms associated with stage II injuries. While the typical orthotic is posted at 4 degrees varus, patients with stage II tibialis posterior injuries respond well to orthotics posted at 6 degrees or more.
Fig. 1. Manipulation to restore forward glide of the calcaneus beneath the talus. In this adjustment, the plantar heel is stabilized by friction from the examining table while the crossed thumbs apply a posterior shear force through the talus. Initially, a force is applied gently, causing the talus to glide posterior on the fixated calcaneus. When performed properly, a smooth gliding motion should be felt, and the forefoot should lift slightly off the examining table. This manipulation should be performed with as little force as possible to avoid stressing the tibialis posterior tendon.
Nonoperative treatment for first- and second-stage tendon dysfunction consists of either stock or custom-made orthotics manufactured with large varus posts. The orthotic shell is usually made from soft materials, because patients with tibialis posterior tendinitis often find the harder shells uncomfortable (perhaps because the weakened tibialis posterior is unable to prevent the midfoot from jamming into the orthotic shell). A large varus post is essential, as it effectively reduces symptoms associated with stage II injuries. While the typical orthotic is posted at 4 degrees varus, patients with stage II tibialis posterior injuries respond well to orthotics posted at 6 degrees or more.
In many cases, individuals with stage II tibialis posterior tendinitis present with limited ranges of ankle dorsiflexion. Because restricted ankle dorsiflexion can cause the arch to collapse even farther during propulsion (which greatly strains the tibialis posterior tendon), it is important to maintain ankle mobility. The adjustment illustrated in figure 1 is often helpful when maintaining ankle dorsiflexion.
In addition to orthotics and manipulation, strengthening exercises should be prescribed. Because tibialis posterior tendon dysfunction is often associated with excessive dorsiflexion of the first metatarsal following heel lift, it is important to exercise the peroneus longus (Fig. 2). Most importantly, to prevent continued deformity, it is essential that the tibialis posterior muscle itself be strengthened.
Although numerous exercise protocols have been recommended, a detailed pre- and post-MRI study of tibialis posterior activity associated with specific exercises confirms that forefoot adduction resisted by elastic bands produces the greatest increase in activity. In fact, compared to conventional heel-raise exercises, resisted adduction produced almost twice as much activity in the tibialis posterior muscle.3
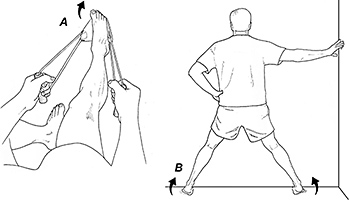 Fig. 2. Peroneus longus home exercises. A simple peroneus longus exercise is performed by plantarflexing and everting the forefoot against resistance from an elastic band (A). A more advanced peroneus longus exercise is performed by standing with hips abducted and knees flexed while plantarflexing and everting the ankles (B).
When combined with orthotics and various manual techniques to maintain ankle range of motion, tibialis posterior strengthening exercises produce significant reductions in pain and improve function in individuals with stage I and II tibialis posterior tendon dysfunction. The efficacy of this approach was demonstrated in a randomized, controlled trial by Kulig, et al.4 Using a specially designed exercise device to apply eccentric resistance to the tibialis posterior in the transverse plane, these authors demonstrated that a combined treatment of eccentric exercises and orthotics in the management of stage I and II tibialis posterior tendon dysfunction produces significant reductions in pain and disability, compared to orthotics and stretching alone.
Fig. 2. Peroneus longus home exercises. A simple peroneus longus exercise is performed by plantarflexing and everting the forefoot against resistance from an elastic band (A). A more advanced peroneus longus exercise is performed by standing with hips abducted and knees flexed while plantarflexing and everting the ankles (B).
When combined with orthotics and various manual techniques to maintain ankle range of motion, tibialis posterior strengthening exercises produce significant reductions in pain and improve function in individuals with stage I and II tibialis posterior tendon dysfunction. The efficacy of this approach was demonstrated in a randomized, controlled trial by Kulig, et al.4 Using a specially designed exercise device to apply eccentric resistance to the tibialis posterior in the transverse plane, these authors demonstrated that a combined treatment of eccentric exercises and orthotics in the management of stage I and II tibialis posterior tendon dysfunction produces significant reductions in pain and disability, compared to orthotics and stretching alone.
Since the device used in this study is not commercially available, the tibialis posterior exercise illustrated in figure 3 is recommended. Because the degree of tendon damage in stage II deformities varies greatly, care must be taken when prescribing home exercises for these patients, and their form and symptoms must be monitored carefully.
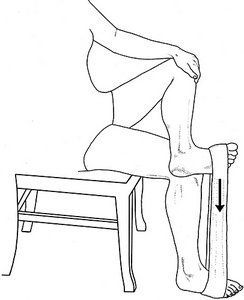 Fig. 3. Tibialis posterior home exercise. With the involved foot placed over the opposite knee, an elastic band is positioned between the forefeet so tension from the band pulls the involved upper forefoot downwardly. This position allows the patient to perform eccentric load exercises by lifting the involved forefoot by hand (to avoid the concentric phase) while using tibialis posterior to actively lower the involved forefoot during the eccentric phase. The eccentric portion of the exercise should last 3 seconds and the patient typically performs three sets of 15 repetitions daily.
For difficult stage II cases, many practitioners prescribe the Richie brace. This popular brace was designed to limit frontal plane motion of the rearfoot while allowing an orthotic to be worn inside the brace. Because it allows the foot to move in the sagittal plane, this brace is less likely to produce the reductions in strength and bone density associated with typical walking boots.
Fig. 3. Tibialis posterior home exercise. With the involved foot placed over the opposite knee, an elastic band is positioned between the forefeet so tension from the band pulls the involved upper forefoot downwardly. This position allows the patient to perform eccentric load exercises by lifting the involved forefoot by hand (to avoid the concentric phase) while using tibialis posterior to actively lower the involved forefoot during the eccentric phase. The eccentric portion of the exercise should last 3 seconds and the patient typically performs three sets of 15 repetitions daily.
For difficult stage II cases, many practitioners prescribe the Richie brace. This popular brace was designed to limit frontal plane motion of the rearfoot while allowing an orthotic to be worn inside the brace. Because it allows the foot to move in the sagittal plane, this brace is less likely to produce the reductions in strength and bone density associated with typical walking boots.
Referral Considerations
Although stage I and II deformities typically respond well to conservative care, stage III and IV tendon deformities are less predictable and surgical intervention is often required. If deformity of the foot progresses despite conservative treatment, various surgical interventions may be necessary, such as flexor digitorum longus tendon transfer, calcaneal osteotomy, lateral column lengthening and/or heel cord lengthening.5
Stage III / IV deformities are characterized by fixed flatfoot deformities, in which patients are unable to invert their heels even a few degrees during static stance. The extreme weakness of tibialis posterior secondary to degeneration and elongation makes a single-leg heel raise impossible. The rearfoot is fixed in valgus and patients are apropulsive during the gait cycle. Stage IV is differentiated from stage III by the presence of pain and/or crepitus with tibiotalar motion.
According to Gluck, et al.,5 treatment for painful stage III tibialis posterior tendon disorders should include a prescription of a rigid ankle-foot orthosis and consideration of triple arthrodesis. Because of ankle involvement, stage IV deformity may require tibiotalocalcaneal arthrodesis or triple arthrodesis with total ankle arthroplasty.
References
- Bloome DM, Marymont J, Varner K. Variations on the insertion of the posterior tibialis tendon: a cadaveric study. Foot Ankle Int, 2003 Oct;24:780-783.
- Houck J, Neville C, Tome J, et al. Foot kinematics during bilateral heel rise test in participants with stage 2 posterior tibial tendon dysfunction. J Orthop Sports Phys Ther, 2009;39:593.
- Kulig K, Burnfield J, Requejo S, et al. Selective activation of tibialis posterior: evaluation by the magnetic resonance imaging. Med Sci Sports Exerc, 2004:867.
- Kulig K, Reischl S, Pornrantz A, et al. Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive exercise: a randomized controlled trial. Phys Ther, 2009;89:1-11.
- Gluck G, Heckman D, Parekh S. Tendon disorders of the foot and ankle, part 3. The posterior tibial tendon. Am J Sports Med, 2010;38:2133.
Click here for more information about Thomas Michaud, DC.





