Editor's Note: Part 1 of this article addressed when and why to order an MRI (Jan. 15 issue).
As I wrote in my previous article on this topic, it is my goal for you, the doctor, to be an expert in interpreting MRI images yourself; and to be able to independently make decisions based upon a combination of clinical presentations and findings, followed by the MRI images.
When considering utilizing the MRI as a diagnostic tool, never lose sight of the fact that the MRI images are no more important than any other diagnostic tool inclusive of your clinical examination. Your clinical examination is both what helps determine if the MRI is clinically indicated and corroborates your clinical findings. Only then can you make a final diagnosis regarding a disc (or any other space-occupying lesion) as the cause of your patient's pain.
Can You Help? MRI Findings and Whether to Refer or Treat
Once you have determined a conclusive diagnosis based upon the MRI images, the next decision in the triage process is whether you can help the patient, which is followed by what to do. In our world, it is diagnosis, prognosis, treatment plan ... then treat the patient. In this scenario, the MRI can be the missing piece in establishing a conclusive diagnosis.
 Should your clinical examination reveal significant radiculopathic or myelopathic findings (versus the absence of both), it could change how you triage the care of your patient. A radiculopathic finding is any motor or sensory aberration in the limbs or radiating around the flanks inclusive of aberrant reflexes, foot drop, sensory deficit or hyperesthesia – in short, anything that can be affected at the root level from both the anterior and posterior horn innervations. A myelopathy is cord compression with ensuing neurological deficit distal to the level of the lesion. The presence of either (significant) finding raises the question of what I term real estate.
Should your clinical examination reveal significant radiculopathic or myelopathic findings (versus the absence of both), it could change how you triage the care of your patient. A radiculopathic finding is any motor or sensory aberration in the limbs or radiating around the flanks inclusive of aberrant reflexes, foot drop, sensory deficit or hyperesthesia – in short, anything that can be affected at the root level from both the anterior and posterior horn innervations. A myelopathy is cord compression with ensuing neurological deficit distal to the level of the lesion. The presence of either (significant) finding raises the question of what I term real estate.
Understanding "Real Estate" in the Context of MRI Findings
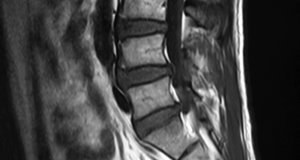
The "real estate" of a space-occupying lesion in the form of a herniated or bulging disc (degeneration or from alteration of motion segment integrity) is the region between the disc and the neurological element. If there is adequate space evidenced by cerebral spinal fluid, the likelihood of your patient responding favorably to chiropractic care is much greater.
Should the space be compromised with a space-occupying lesion, you should consider a consultation with either a neurosurgeon or orthopedic surgeon who has done a fellowship in neuro-spine. I strongly suggest you avoid any orthopedic surgeons who are general orthopedists, as they lack the advanced spine surgical training, and it has been my 35-plus-years' experience that neurosurgeons or neuro-spine-trained orthopedists have better outcomes.
In triaging the care of your patient, you also must identify if the disc is causing an abutment of the root or cord, or a compression. An abutment is when you have only one side of the neural element making contact; usually the disc on the anterior component of the cord or the nerve root. With an abutment, you have much more leeway, as there is adequate space on the opposing side, while compressions give you little room to work with.
In addition, inherently the adjustment causes an increase in intrathecal pressure and could momentarily expand the disc on the neurological element, possibly having a neurological negative sequella.
There are many chiropractic techniques taught today to manage the disc patient, with decompression one modality the DC can utilize. With decompression, many proponents have reported significant improvement in both scenarios, although I have not read any literature to verify that. However, in spite of the lack of literature, I would follow the same protocols in determining if there is enough "real estate" available, and if not, co-manage the patient with a spine surgeon who understands your treatment and goals. This would appear to be in the best public interest, while concurrently reducing both the doctor's and patient's risk.
When considering ipsilateral pain with contralateral lesions (disc herniated on one side and pain on the opposite side), we must consider four possible etiologies:
- Traction generated from the nerve roots2
- Hypertrophy of asymmetrical ligamenta flava3
- Central hyerexcitability of the dorsal rami4
- Increased pressure from fluid in a closed spinal region5
However, in this scenario, the same rules apply once you have concluded an accurate diagnosis of the cause of the historical and clinical findings. If there is enough "real estate," then consider treating without a surgical consultation; if there isn't, consider seeking another opinion.
Bed Rest and Non-Force Techniques
One significant treatment modality most overlooked in our profession is bed rest. Many experienced neurosurgeons often utilize this treatment protocol, as the disc does desiccate, or dry up and shrink, to some degree in a short amount of time. The goal is to allow the disc to recede from the nerve enough to gain valuable "real estate," no matter how minimal, and a clinical evaluation will let you know if the nerve has decompressed enough to adjust your patient, lowering the risk of negative sequellae. Non-force techniques such as sacro-occipital technique, blocking and others work well in conjunction with bed rest and leave little risk while waiting for the disc to desiccate.
Take-Home Points
- The balance in triaging the patient is not to wait too long with a compressed neurological element, which can potentially demyelinate over time, causing other issues.
- Therefore, in treating these acute patients, performing a complete clinical examination, followed by the necessary ordering of MRIs with correct slice thicknesses; being able to interpret them; and then having a surgeon to consult with, becomes integral to the contemporary chiropractic practice. This level of triage has nothing to do with your chiropractic philosophy or treatment method, as 99 percent of chiropractors treat mechanical spine pain (no fracture, tumor or infection).
- In the absence of appropriate training to interpret spinal MRIs, insist (demand) that your images be read only by a neuroradiologist.
References
- Lurie JD, Doman DM, Spratt KF, Tosteson, et al. Magnetic resonance imaging interpretation in patients with symptomatic lumbar spine disc herniations: comparison of clinician and radiologist readings. Spine, 2009;34(7):701-705.
- Suca HK, Gelal F. Lumbar disk herniation with contralateral symptoms. European Spine J, 2006;15(5):570–574.
- Karabekir HS, Yildizhan A, Atar EK, et al. Effect of ligamenta flava hypertrophy on lumbar disc herniation with contralateral symptoms and signs: a clinical and morphometric study. Arch Medical Sci, 2010;6(4):617-622.
- Hirayama J, Yamagata M, Ogata S, et al. Relationship between low-back pain, muscle spasm and pressure pain thresholds in patients with lumbar disc herniation. European Spine J, 2006;15(1):41-47.
- Yi YJ, Kang SS, Yoon YJ, Shin KM. Contralateral complete L5 palsy following ipsilateral L4 selective transforaminal epidural block. Korean J Anesthesiology, 2013;65(6 Suppl), S56–S58.
Dr. Mark Studin is an adjunct associate professor at the University of Bridgeport School for Chiropractic, teaching advanced imaging and triaging chronic and acute patients; and an adjunct postdoctoral professor at Cleveland University-Kansas City College of Chiropractic. He is also a clinical instructor for the State University of New York at Buffalo, Jacobs School of Medicine and Biomedical Sciences, Office of Continuing Medical Education. Dr. Studin consults for doctors of chiropractic, medical primary care providers and specialists, and teaching hospitals nationally. He can be reached at
or 631-786-4253.




