Einstein is purported to have said, "When a man sits with a pretty girl for an hour, it seems like a minute. But let him sit on a hot stove for a minute and it's longer than any hour. That's relativity." In some way, everything is relative to one's point of view.
Paternalism: Forgetting Your Duty to Educate Patients
So, as a parent enforces upon their children certain mandates for the child's best interest (e.g., "You must eat your fruits and vegetables"), doctors believed anything that would get a patient to do what the doctor believed was best was OK.
In the past, this went as far as misleading a patient by directing them toward the best treatment. From the doctor's point of view, patients could not be trusted with making intelligent decisions about their own health care. Evidence-based practice (EBP) is based upon the three-legged stool of best available research, doctor expertise and patient values. Thus, EBP acknowledges the central role the patient plays in determining what treatments they should undergo.
When I was a child, my father would use that Einstein quote to suggest if you can't explain something difficult such that any person can understand it, then you don't really understand it.
 Figure 1: Making the Complex Understandable: Low back pain, no exercise.
I've read two studies that used graphic devices to help educate patients about the probabilities of various outcomes for their health in ways that are easier to understand than giving them hard-to-interpret statistics such as odds ratios, effect sizes and NNT (number needed to treat), even if these are used to create the graphical elements the patients are shown.1-2
Figure 1: Making the Complex Understandable: Low back pain, no exercise.
I've read two studies that used graphic devices to help educate patients about the probabilities of various outcomes for their health in ways that are easier to understand than giving them hard-to-interpret statistics such as odds ratios, effect sizes and NNT (number needed to treat), even if these are used to create the graphical elements the patients are shown.1-2
For example, using data from Hides, et al.,3 one can create, with a free Java app,4 images that illustrate the effects of teaching abdominal hollowing exercises (a transversus abdominis exercise that causes co-contraction of the multifidi) on preventing a recurrence of the first bout of low back pain. Figure 1 shows that data extracted from that study allow one to predict that in a sample of 100 patients who were successfully treated for their first bout of low back pain, 84 (red unhappy faces) would have a recurrence within a year.
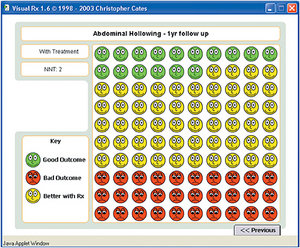 Figure 2: Making the Complex Understandable: Low back pain with exercise.
Figure 2 shows that in those who were taught abdominal hollowing, only 30 (red unhappy faces) should have a recurrence, but the 16 (green faces) who wouldn't have had a recurrence of pain without the exercise still won't. The treatment doesn't affect them for better or worse. But for the 54 people (yellow happy faces) who learned the exercise, doing so appears to prevent the recurrence of LBP.
Figure 2: Making the Complex Understandable: Low back pain with exercise.
Figure 2 shows that in those who were taught abdominal hollowing, only 30 (red unhappy faces) should have a recurrence, but the 16 (green faces) who wouldn't have had a recurrence of pain without the exercise still won't. The treatment doesn't affect them for better or worse. But for the 54 people (yellow happy faces) who learned the exercise, doing so appears to prevent the recurrence of LBP.
A New Problem With Paternalism in Chiropractic
Rather than finding a better way to teach patients – to make things easier for them to understand, so they can make their own choices about their health – there is a new type of paternalism coming from some in our profession: a paternalistic method to get new patients. The idea is that a new patient signs a contract mandating, among other questionable things, that the patient must bring their family in for an examination to determine if the family members have subluxations. The contract stipulates that if the patient does not bring in these family members, the doctor will terminate care.
The rationale presented in these contracts is that it would be "unethical" for the doctor to continue to treat the patient knowing the patient's family members might have uncorrected subluxation.
I am sure the rationale behind this strategy is that one cannot leave a person's family to suffer while they are getting healthier with chiropractic care. Thus, from the doctor's point of view, this way to get a patient to bring their family in to be examined is really being done in the patient's and their family's best interest. In a paternalistic fashion, the chiropractor is forcing the patient to do what the chiropractor thinks is good for the patient's family.
However, if it is unethical for the patient's family to suffer because they won't come to the chiropractor, how is it ethical for the doctor to terminate treatment for the original patient? The doctor has a more compelling moral duty to their current patient than they have to the patient's family, who aren't yet patients.
You might be thinking: That's true, but sometimes patients need encouragement to do the right thing. While it may be done with the best of intentions – making sure the patient's family members get a check-up – to outside observers this is wrong on several levels.
It is coercive to tell a patient in pain the doctor will let you suffer in pain if you don't bring in your family. While the doctor might have an altruistic intent, the ends do not justify the means. Moreover, if the doctor terminates care just because the patient's family members can't or won't come to see the doctor, and the patient still needs care, the doctor risks a malpractice claim of abandonment.
Evidence-Based Health Care and Paternalism: Oil and Water?
Finally, none of this deals with the lack of evidence that finding a subluxation and correcting it will prevent an illness in an otherwise healthy person; and the ethical problem of trying to get the family in for something that the United Kingdom's General Chiropractic Council (GCC) has ruled "is not supported by any clinical research evidence that would allow claims to be made that it is the cause of disease or health concerns." Further, the GCC writes that chiropractors "must make sure their own beliefs and values do not prejudice the patients' care."5
Please keep in mind that the GCC isn't what I have been called – a "subluxation denier." The council (and I) are just acknowledging the current lack of clinical research to document the health-robbing effects some claim for the subluxation.
Looking from a skeptical point of view and being intellectually honest about the state of the evidence are important. Back in the 1940s, C.O. Watkins, DC, then-chairman of the National Chiropractic Association (predecessor of ACA), urged: "Resolve to be bold in what we hypothesize, but cautious and humble in what we claim."
I am happy to report there is a fledgling attempt by those who believe the subluxation theory to develop a research agenda.6 As Nelson wrote 20 years ago: "Whether chiropractors are actually treating lesions, or not, is a question of immense clinical and professional consequence. Resolution of the controversy will not be found through consensus panels nor through semantic tinkering, but through proposing and testing relevant hypotheses."7
Until we have adequately tested those hypotheses and either provided evidence to support them or evidence that doesn't support them, we will be judged by how we use these hypotheses. The morality of our behavior will be judged relative to different points of view, not just ours. Others will judge the morality of an action, such as requiring a patient to bring their family in for a subluxation check-up as a requirement of caring for one member of the family.
Looking at the morality of the action from only our point of view is paternalistic. We need to keep in mind that patients have the right to decide – without paternalistic coercion – what they want to do.
When Assendelft, et al.,8 published their meta-analysis on spinal manipulative therapy for LBP in 2003, I heard from many critics on a health fraud mailing list that there was no longer a need for chiropractors, as the study concluded (if one only read the abstract): "There is no evidence that spinal manipulative therapy is superior to other standard treatments for patients with acute or chronic low back pain." However, the body of the paper presented a more nuanced conclusion that the treatments were of equal effectiveness and were both available options.
I argued to the critics that given an equal outcome, patients had the right to choose between manipulation and medication; the paternalistic approach was that the only option was medication. That approach is just as wrong and as paternalistic as trying to force a patient's family into receiving chiropractic care just because from the chiropractor's point of view, it is the best treatment method. Paternalism has no place in evidence-based health care.
References
- Fagerlin A, Wang C, Ubel PA. Reducing the influence of anecdotal reasoning on people's health care decisions: is a picture worth a thousand statistics? Med Decis Making, 2005 Jul-Aug;25(4):398-405.
- Hoffman JR, Wilkes MS, Day FC, Bell DS, Higa JK. The roulette wheel: an aid to informed decision making. PLoS Med, 2006 Jun 13;3(6):e137.
- Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine, 2001 Jun 1;26(11):E243-8.
- VisualRx: www.nntonline.net/visualrx/introduction.
- Guidance on Claims for Vertebral Subluxation Complex. General Chiropractic Council, U.K., May 2010.
- McCoy M, Kent C. Vertebral subluxation research: an agenda to explore the epidemiology of vertebral subluxation and the clinical outcomes related to management. J Vertebral Subluxation Res, 2013 Aug 5;:29–32.
- Nelson CF. Chiropractic scope of practice. J Manip Physiol Ther, 1993 Sep;16(7):488–97.
- Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. A meta-analysis of effectiveness relative to other therapies. Ann Int Med, 2003 Jun 3;138(11):871–81.
Click here for previous articles by Stephen M. Perle, DC, MS.





