Author's Note: The rising tide of both research and public awareness in stress-related issues understandably points our attention to the brain and central nervous system. Accordingly, it is of special interest to the chiropractic profession to be aware of the interconnectedness of the musculoskeletal, immune and hormonal systems, among others.
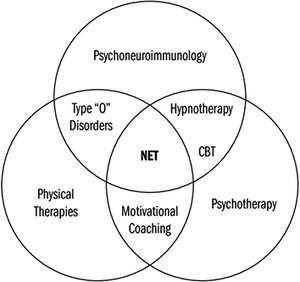 The interrelationship between physical therapies, psychological therapies, and psychoneuroimmunology. Type O disorders are non-mechanical conditions which replicate the symptoms of common musculoskeletal disorders. CBT refers to cognitive behavioral therapy.
Extending the concepts of biopsychosocial medicine and cognitive behavioral therapy to resolve pain (as described in my previous article), the Neuro Emotional Technique (NET) was introduced as a multimodal intervention originally based upon three essential concepts:1
The interrelationship between physical therapies, psychological therapies, and psychoneuroimmunology. Type O disorders are non-mechanical conditions which replicate the symptoms of common musculoskeletal disorders. CBT refers to cognitive behavioral therapy.
Extending the concepts of biopsychosocial medicine and cognitive behavioral therapy to resolve pain (as described in my previous article), the Neuro Emotional Technique (NET) was introduced as a multimodal intervention originally based upon three essential concepts:1
Cognitive Behavioral Psychology: NET seeks the reversal or extinction of classically conditioned distressing emotional responses to trauma-related stimuli, such as challenges to our status, demands for performance, or other situations in which a perceived stimulus exceeds immediate coping ability – all of which produce stress. NET does not involve any type of psychotherapy or "talking it out" therapy.
Traditional Chinese medicine: NET engages the energy system, in that a patient touches a pulse point that is determined to be involved in the body's stress reaction to a particular stimulus. Correlating the emotions to the meridian system has been expressed in acupuncture theory for 2,000 years.2 Current concepts hold that tightness in the fascial system might represent acupoints and meridians in the human body.3
Muscle Testing: This feedback technique is believed to be an indicator of altered physiological function, in which a given muscle is less capable of resisting an outside force when there is some alteration in the function of the nervous system.4 Specifically, it was proposed that the muscle test responds to cognitive and emotional stimuli.5
The effectiveness of NET was explained in other terms as the "neuromatrix," a neurological signature triggered when pain is perceived, called the Neuro Emotional Complex (NEC). With prolonged stimulation over time, less sensory input is needed to produce pain sensation; i.e., the neuromatrix has become sensitized.6 Furthermore, pain sensations may persist long after the removal of the original pain producing injury or stimulus.7
Physical therapies in themselves may include elements of spinal manipulation, physiotherapy and massage. Emotional interventions include the range of mind therapies from simple interrogation to counseling. Portions of these two approaches are a part of NET. But there is yet another component to NET that underlies these interventions.
Stress and Neurochemical Change
This involves the vast network of chemical events that accompany stressful events, even to the extent that when the stressor is no longer present, the recollection of the past stress response is sufficient to recreate the same chemical conditions in the body.8 In other words, the neurochemical change that occurs in stress has a lasting effect upon patients that has the potential to hinder the patient's ability to resolve current health issues.1
The chemical carriers of this information are known as cytokines and neuropeptides, the latter exemplified by glucagon-like peptide-1 and outer-membrane porin, as well as their receptors.9 Recognized as informational molecules, these small proteins carry complex messages throughout the body. Should a link exist between chronic low back pain and emotional stress, it is likely that these chemical messengers are a vital component of that link.
The fact that significant concentrations of neuropeptides have been found in the brain, spinal cord and immune systems lends noteworthy support to this theory.10
Another Element: Immune Function
Still another element in NET is immune function. Beginning with Ader and Cohen's demonstration that immune reactions could be conditioned,11 the study of interactions among behavioral, neural, endocrine, and immune function was launched as a coalition of these processes, called psychoneuroimmunology (PNI). This established the principle that the nervous and immune systems are components of an integrated system of adaptive processes, creating a paradigm shift in which these systems were no longer viewed in isolation.12
In particular, PNI has been applied to understanding disease processes in greater detail, such that it has focused on the use of immune markers and pro-inflammatory proteins known as cytokines as indicators of immune status, and therefore addressing the state of health.
Like the stress response, the inflammatory reaction is a crucial element of survival and meant to be tailored to the stimulus and time. A full-fledged systematic inflammatory reaction leads to the stimulation of four major programs: 1) the acute phase reaction, 2) the sickness syndrome, 3) the pain program, and 4) the stress response – mediated by the hypothalamic-pituitary-adrenal axis and the sympathetic nervous system.
Indeed, over the past 20 years, numerous studies have documented complex interactions between the brain, immune system and systemic inflammation.13 With NET, therefore, we now can couple those interactions to pain and chronic stress. Portions of all these elements are blended together as shown by the Venn diagram (Fig. 1).
Progressive Evidence-Based Medicine
An important element of NET is its recognition of the most progressive elements of evidence-based medicine. What once began as a slavish adherence to the peer-reviewed literature as the only criterion for what constituted rigorous medical "evidence," there has been an inexorable march to a tripartite model – first consulting the peer-reviewed literature, then incorporating the expertise and clinical judgment of the physician,14 and then finally embracing the expectations and values as emotional components of the individual patient.15
In concrete terms, it is therefore possible to demonstrate that the patient's emotions are a major factor in determining clinical and functional outcomes in patients with low back pain caused by disc herniations.16-17 NET addresses these emotions directly with the prospect of enhancing meaningful outcomes in therapy.
Editor's Note: Dr. Rosner's next article will describe the body of research that supports the clinical efficacy of NET; as well as the nonprofit foundation that has sponsored further research and education regarding this unique, multifactorial approach to chiropractic care.
References
- Walker S. Neuro Emotional Technique seminar manual. Encinitas, CA, 2006.
- Chase CR. The Geometry of Emotions: Using Chakra acupuncture and 5-Phase Theory to describe personality archetypes for clinical use. Med Acupunct, 2018;30:167-78.
- Bai Y, et al. Review of evidence suggesting that the fascia network could be the anatomical basis for acupoints and meridians in the human body. Evid Based Complement Alternat Med, 2011;2011:260510.
- Goodheart GJ. Applied Kinesiology research manuals. Detroit, MI: Private, 1964-1995.
- Walker S. "Ivan Pavlov, His Dog and Chiropractic." Digest Chiro Econ, 1992;34:36-46.
- Melzack R. Pain and the neuromatrix in the brain. J Dent Educ, 2001;65:1378-82.
- Moseley GL. A pain neuromatrix approach to patients with chronic pain. Man Ther, 2003;8:130-40.
- Hanada T, Yoshimura A. Regulation of cytokine signaling and inflammation. Cytokine Growth Factor Rev, 2002;13:413-21.
- Pert CB, et al. Neuropeptides and their receptors: a psychosomatic network. J Immunol, 1985;135:820s-6s.
- Pert CB. The Molecules of Emotion: Why We Feel the Way We Feel. New York, NY: Scribner, 1997.
- Ader R, Cohen N. Behaviorally conditioned immunosuppression. Psychosom Med, 1975;37:333-40.
- Ader R. On the development of psychoneuroimmunology. Eur J Pharmacol, 2000;405:167-76.
- Khandaker GM, et al. Inflammation and immunity in schizophrenia: implications for pathophysiology and treatment. Lancet Psychiatry, 2015;2:258-70.
- Sackett DL. Evidence-based medicine. Semin Perinatol, 1997;21:3-5.
- Sackett D, et al. Evidence-based Medicine: How to Practice and Teach EBM. Edinburgh, Scotland: Churchill Livingstone, 2000.
- Weinstein JN, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Outcomes Research Trial (SPORT): a randomized trial. J Am Med Assoc, 2006;296:2441-50.
- Weinstein JN, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Outcomes Research Trial (SPORT): observational cohort. J Am Med Assoc, 2006;296:2451-9.
Click here for previous articles by Anthony Rosner, PhD, LLD [Hon.], LLC.





