With chiropractic backgrounds rooted in motion palpation and functional rehabilitation, we have observed that the upper-thoracic spine may be the most commonly restricted area in the locomotor system. This restriction of multiple segments (C7-T5) is likely related to cervical disc herniations; degenerative changes at the lower cervical spine; shoulder impingement and rotator-cuff pathologies; and low back pain.
In Len Faye's classic text, Motion Palpation and Chiropractic Technique, the distinction between primary and secondary fixations is made. Primary fixations usually present the most significant restrictions in the locomotor system and should take priority over other fixations, no matter where patients express pain.1 We conclude, based on our years of treating patients, that primary restrictions frequently show up at the cervical-thoracic joint and other transitional areas of the spine. All editions of Karel Lewit's text Manipulative Therapy in Rehabilitation of the Locomotor System support this view.2
Biomechanical Underpinnings and Kinesiopathology
 Figure 1: Forward head posture - upper-crossed syndrome. A = correct; B = incorrect.
The thoracic spine represents a critical, yet underappreciated spinal region.10 Of all structures, the thoracic spine is one of the most vulnerable in modern lifestyles. In the fetal posture, the entire spine is kyphotic. We are hard-wired to achieve a stable, upright posture by 4 years of age,3 yet due to television, soft couches, chairs, desks, computers, etc., the thoracic spine slips back into greater kyphosis. The result: straightening of the lower cervical lordosis with compensatory C0-C1 hyperextension, as the eyes must peer horizontally. In the lumbar spine, we find poor control of the natural lordosis with resultant disc vulnerability during activities of daily living, such as sitting, bending, twist, lifting, etc.
Figure 1: Forward head posture - upper-crossed syndrome. A = correct; B = incorrect.
The thoracic spine represents a critical, yet underappreciated spinal region.10 Of all structures, the thoracic spine is one of the most vulnerable in modern lifestyles. In the fetal posture, the entire spine is kyphotic. We are hard-wired to achieve a stable, upright posture by 4 years of age,3 yet due to television, soft couches, chairs, desks, computers, etc., the thoracic spine slips back into greater kyphosis. The result: straightening of the lower cervical lordosis with compensatory C0-C1 hyperextension, as the eyes must peer horizontally. In the lumbar spine, we find poor control of the natural lordosis with resultant disc vulnerability during activities of daily living, such as sitting, bending, twist, lifting, etc.
Having a stiff upper-thoracic spine also decreases our ability to activate the deep neck flexors and even the abdominals. With freely moveable vertebrae in this junctional area, we are able to achieve balance between the extensors and deep neck flexors, which ironically, originate in the mid- to upper-thoracic region.3
 Figure 2: Internally rotated arms.
We know that with cervical rotation, we should appreciate motion all the way down to T4. Typically, patients with this restriction do not lose much active range of motion. It has been demonstrated that a significant association exists between decreased mobility of the thoracic spine and the presence of patient-reported complaints associated with neck pain.7 Cleland showed that in select patients, thoracic spine manipulation provided a successful treatment for patients with neck pain. Thoracic spine mobilization or manipulation acted as a component of a multi-modal intervention demonstrated to be effective for the treatment of patients with shoulder impingement syndromes.8-9 In a controlled study, this treatment was determined effective by itself.4
Figure 2: Internally rotated arms.
We know that with cervical rotation, we should appreciate motion all the way down to T4. Typically, patients with this restriction do not lose much active range of motion. It has been demonstrated that a significant association exists between decreased mobility of the thoracic spine and the presence of patient-reported complaints associated with neck pain.7 Cleland showed that in select patients, thoracic spine manipulation provided a successful treatment for patients with neck pain. Thoracic spine mobilization or manipulation acted as a component of a multi-modal intervention demonstrated to be effective for the treatment of patients with shoulder impingement syndromes.8-9 In a controlled study, this treatment was determined effective by itself.4
 Figure 3: Respiration. A = Normal; B = faulty.
Acting as the compensating machines that we are, we develop hypermobile segments in the lower cervical spine when faced with upper-thoracic spine restrictions. Here, simple engineering principles apply. We have vertebrae in our spine designed to provide us movement at every segment in all three planes of motion (transverse, coronal, sagittal). If this were not the case, we would have a solid column of bone to protect our spinal cord; instead, the spine is segmented and designed for controlled motion. When motion is restricted in this key transitional area, we force rotation into segments that are not designed for this task. This leads to breakdown.
Figure 3: Respiration. A = Normal; B = faulty.
Acting as the compensating machines that we are, we develop hypermobile segments in the lower cervical spine when faced with upper-thoracic spine restrictions. Here, simple engineering principles apply. We have vertebrae in our spine designed to provide us movement at every segment in all three planes of motion (transverse, coronal, sagittal). If this were not the case, we would have a solid column of bone to protect our spinal cord; instead, the spine is segmented and designed for controlled motion. When motion is restricted in this key transitional area, we force rotation into segments that are not designed for this task. This leads to breakdown.
In younger patients, we find acute cervical disc herniations most commonly at C5-C6 and C6-C7. As we age, the body does a clever thing. It will lay down bone or osteophytes in an attempt to stabilize this area of hypermobility. This is a normal response for a poorly functioning kinematic system. The problem these bony outgrowths or osteophytes present is that while they do solve the hypermobility problem, they often leave the patient with narrow IVF canals or spinal stenosis.
 Figure 4: The T4 wall slide.
As chiropractors, we pride ourselves on treating the source of pain, not the symptoms. The true source of musculoskeletal strain in the cervical or lumbar spine or shoulder girdle is upper-thoracic spine stiffness. Of course, as the patient approaches the end of this spectrum of joint dysfunction, adjunct therapy might be necessary (epidural steroid injections, surgery, etc.) For long-term symptom relief, rooting of the cause is paramount.
Figure 4: The T4 wall slide.
As chiropractors, we pride ourselves on treating the source of pain, not the symptoms. The true source of musculoskeletal strain in the cervical or lumbar spine or shoulder girdle is upper-thoracic spine stiffness. Of course, as the patient approaches the end of this spectrum of joint dysfunction, adjunct therapy might be necessary (epidural steroid injections, surgery, etc.) For long-term symptom relief, rooting of the cause is paramount.
Later on, we'll detail the causative factors for upper-thoracic spine restriction, what palpations and functional tests can be performed to confirm this dysfunction, and treatment concepts and considerations.
Assessment Protocols
The masters of manual therapy are able to marry what they find with their hands through palpation with what they see with their eyes through movement analysis or functional screening. With finely tuned dynamic palpation skills, the physician is able to palpate joint restriction, joint hypermobility and soft-tissue pathology. As Karel Lewit once said, "The human hand is the greatest therapeutic tool that has [been] or ever will be invented." The purpose of functional assessment is to identify a patient's functional or performance deficits and capabilities. Structural problems, such as disc herniations or arthritis are noted but not over-emphasized to the patient.
 Figure 5: Squat with kyphosis.
As the physician takes the patient through dynamic palpation and functional assessment, the cause of the patient's pain becomes apparent. Often, we will see or suspect a dysfunction of the upper-thoracic spine with a dysfunctional T4 wall slide or failed squat pattern (Figures 4, 5). These tests will give us "soft findings," as the exact locomotor culprit is still unknown. Our suspects would include lack of thoracic spine extension, tight latissimus dorsi, tight pectoralis major and minor, and poor postural stabilization of the diaphragm. Further testing should include upper-thoracic spine joint play (Figure 8), latissimus length testing, pectoralis length testing and Kolar postural diaphragm testing.
Figure 5: Squat with kyphosis.
As the physician takes the patient through dynamic palpation and functional assessment, the cause of the patient's pain becomes apparent. Often, we will see or suspect a dysfunction of the upper-thoracic spine with a dysfunctional T4 wall slide or failed squat pattern (Figures 4, 5). These tests will give us "soft findings," as the exact locomotor culprit is still unknown. Our suspects would include lack of thoracic spine extension, tight latissimus dorsi, tight pectoralis major and minor, and poor postural stabilization of the diaphragm. Further testing should include upper-thoracic spine joint play (Figure 8), latissimus length testing, pectoralis length testing and Kolar postural diaphragm testing.
Proper respiration and postural stabilization is provided by the diaphragm. When the diaphragm serves as the primary muscle for respiration, the auxiliary muscles of respiration are able to remain soft and relaxed. Many of our patients who have upper-thoracic spine restriction will dominate breathing with the scalenes and upper scapula fixators. If the patient is able to breathe properly, every breath is a natural mobilization to all the spinal joints, costovertebral joints and sternoclavicular joints. The diaphragm is also crucial for stabilizing the lumbar spine through IAP (see Figure 3 for respiration screen).
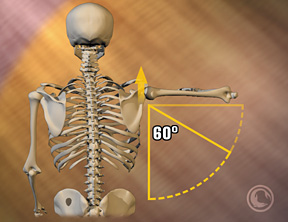 Figure 6: Arm abduction (after Janda).
Joint fixation can occur due to internal or external causes. Internal causes include improper stabilization of the upper extremity. Often patients will dominate arm movement with the upper trapezius and levator scapula. This coincides with muscular inhibition of the serratus anterior and lower and middle trapezius. Essentially, the patient is overusing the neck musculature to move the upper extremity. This can be correlated with Janda's arm abduction screen (Figure 6) and Janda's trunk-lowering test (Figure 7).12
Figure 6: Arm abduction (after Janda).
Joint fixation can occur due to internal or external causes. Internal causes include improper stabilization of the upper extremity. Often patients will dominate arm movement with the upper trapezius and levator scapula. This coincides with muscular inhibition of the serratus anterior and lower and middle trapezius. Essentially, the patient is overusing the neck musculature to move the upper extremity. This can be correlated with Janda's arm abduction screen (Figure 6) and Janda's trunk-lowering test (Figure 7).12
This strategy, which is detrimental to the cervical spine, will also lead to shoulder girdle dysfunction. Over time, this improper synergy of muscle activity will cause a predictable pattern of upper-thoracic joint dysfunction.
 Figure 7: Faulty trunk-lowering test (after Janda).
We often hyperfocus as chiropractors, treating only the joint fixation through adjustments and mobilizations without addressing the related faulty movement pattern. Keep in mind that practitioners should still manipulate this area as warranted, as adjustments have been proven to provide effective treatment in this region.5-6 Clinical experience would suggest that adjustments in this area will facilitate any upper-thoracic spine rehab program. Given that external causes of upper-thoracic spine fixation include improper posturing or trauma, simply sitting in a slouched posture throughout the day can drive upper-thoracic spine restriction.
Figure 7: Faulty trunk-lowering test (after Janda).
We often hyperfocus as chiropractors, treating only the joint fixation through adjustments and mobilizations without addressing the related faulty movement pattern. Keep in mind that practitioners should still manipulate this area as warranted, as adjustments have been proven to provide effective treatment in this region.5-6 Clinical experience would suggest that adjustments in this area will facilitate any upper-thoracic spine rehab program. Given that external causes of upper-thoracic spine fixation include improper posturing or trauma, simply sitting in a slouched posture throughout the day can drive upper-thoracic spine restriction.
Again, repeated manipulation without addressing proper posture will usually not produce long-standing results with treatment. A one-time traumatic event can be the culprit in upper-thoracic dysfunction; however, cumulative microtrauma, as mentioned above, is the more common cause.
The examination begins with a postural evaluation. Findings related to upper-thoracic spine dysfunction include the following:
Posture
- Forward head posture (ears forward of the acromion) (Figure 1)
- Rounded shoulders with internally rotated arms due to shortening of pecs, latissimus dorsi or subscapularis (Figure 2)
Functional Tests
Improper respiration (Figure 3)
- Fail if cephalad movement of rib cage with inspiration; holding in of the abdominal region; insufficient lateral expansion of the lower ribs
- Ideal pattern involves greater degree of horizontal (360°) than vertical motion
T4 wall slide (Figure 4); fail if:
- Arms can't touch wall in a supinated position (tight pecs and other shoulder girdle internal rotators)
- Anterior rib cage lifted (oblique diaphragm due to T/L junction hyperextension and failure of oblique abdominal slings to centrate the rib cage)
- Failure to centrate C0-C1 junction or bring lumbar spine to within 1 inch of the wall due to a fixed thoracic kyphosis
Squat Pattern (Figure 5)
- Fail if loss of lumbar lordosis
- Normal: ability to squat below horizontal with good form (neutral lordosis, patellofemoral stability)
- Ideal: ability to squat with arms overhead as per Cook's Functional Movement Screen11
Janda's arm abduction screen (Figure 6)
- Fail if during the "setting phase," first 60 degrees, the shoulder blade elevates
 Figure 8: Upper t-spine joint play assessment.
Janda's trunk lowering test (Figure 7); fail if:
Figure 8: Upper t-spine joint play assessment.
Janda's trunk lowering test (Figure 7); fail if:
- Scapulae retract
- Scapulae wing
- Scapulae shrug
Muscle-Length Tests
- Latissimus length test
- Pectoral length test
Joint-Play Tests
- Upper t-spine extension (Figure 8)
Clinical Application
The T4-8 region is crucial to evaluate in most cases of musculoskeletal pain. Headaches or cervical radiculopathy associated with a forward head posture may be secondary to fixed thoracic kyphosis. Similarly, sciatica associated with loss of control of the neutral lumbar lordotic posture during sitting or bending / lifting / twisting activities may be secondary to fixed thoracic kyphosis. Thus assessment of function of this region in posture and during movement screens such as the squat, arm abduction, respiration, and trunk lowering from a push-up are essential.
The question of prioritizing treatment goals then arises. The direct approach is to mobilize the stiff T4-8 region before working to stabilize the deep neck flexors, deep abdominal wall, etc. This is a fundamental pillar of the Prague School philosophy, which has also found a home in Gray Cook's work.2,11-12 However, it can work just as well to re-educate neuromuscular pathways or patterns for performing a squat or lunge with good form. This will automatically facilitate (i.e., "reboot") the motor program for upright posture. Another alternative is dynamic neuromuscular stabilization from Kolar.3 There is no exact protocol to improve upright posture, but there are predictable muscle-joint relationships and neuromuscular principles to consider.
References
- Faye L Motion Palpation and Chiropractic Technic, 2nd Edition. Huntington Beach: The Motion Palpation Institute, 1990.
- Lewit K. Manipulative Therapy in Rehabilitation of the Locomotor System, 3rd Edition. Boston: Butterworth-Heineman, 1999.
- Kolar P. Facilitation of Agonist-Antagonist Co-activation by Reflex Stimulation Methods. In: Liebenson C. Rehabilitation of the Spine, 2nd Edition. Baltimore: Lippincott/Williams and Wilkins, 2007.
- Boyles RE, Ritland BM, Miracle BM, et al. Man Ther, 2009;14:375-380.
- Cleland JA, Childs JD, McRae M, Palmer JA, Stowell T. Immediate effects of thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther, 2005;10:127-135.
- Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther, 2007;87:9-23.
- Norlander S, Nordgren B. Clinical symp- toms related to musculoskeletal neck- shoulder pain and mobility in the cervico- thoracic spine. Scand J Rehabil Med, 1998;30:243-251.
- Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. Journal of Orthopaedic and Sports Physical Therapy, 2000;30:126-37.
- Bergman GJ, Winters JC, Groenier KH, Pool JJ, Meyboom-de Jong B, Postema K, et al. Manipulative therapy in addition to usual medical care for patients with shoulder dysfunction and pain: a randomized, controlled trial. Annals of Internal Medicine, 2004;141:432-9.
- Liebenson CS. Treatment of mid-thoracic dysfunction: a key link in the body axis. Part 1: overview and assessment. Journal of Bodywork and Movement Therapies, 2001;5(2):90-98.
- Cook G. Movement: Functional Movement Systems. On Target Publications, Santa Cruz, CA: 2010.
- Janda V, Frank C, Liebenson C. Evaluation of Muscle Imbalance. In: Liebenson C. Rehabilitation of the Spine, 2nd Edition. Baltimore: Lippincott/Williams and Wilkins, 2007.





